The hydatid cyst has a predilection to involve the liver and lungs. Most cases of reported intra-pleural hydatid cysts are secondary; primary involvement has rarely been reported in English language literature. Here we report a 14-year-old child who complained of dyspnea, coughing evolving in a context of apyrexia, and conservation of the general state, Primary pleural hydatidosis was suspected on the chest x-ray and the chest CT scan. Thefore the patient received surgical drainage with emission of false membranes through the chest tube, albendazole was a administered postoperatively for 6 months. During this period, liver function tests results were normal. The primary pleural location of the hydatid cyst is very rare or even exception eland his discovery is often fortuitous. Imaging has a fundamental role in its management. Indeed, it makes it possible to evoke the diagnosis, to specify the topography and Hto look for other localizations.
Echinococcosis, Pulmonary, Hydatid cyst, Pleura
Hydatidosis is a parasitic disease caused by the developmentin humans of the larval form of Echinococcus Granulosus, a small dog tapeworm. Pleural localization is extremelyrare even in endemic countries and represents only 1.3% of thoracic locations [1]. In front of the discretionclinical symptomatology and nonspecificityits radiological appearance, the cysthydatid poses a diagnostic problem withother pleural cystic locations andparietal. We report an observation (primitive pleural hydatid cyst) by insistingon the fundamental place of different imaging techniques in diagnosis.
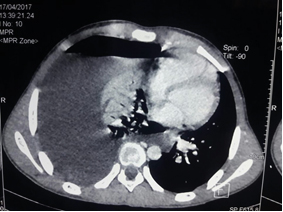
14-year-old boy, with no pathological history and no notion of contact with dogs, reported since 3 months right thoracic pain, chest tightness, evolving in a context of apyrexia, and conservation of the general state. The clinicalexamination revealed a right fluid effusion syndrome. In the general presentation, the patient was hemodynamically stable, with a pulse rate of 80 beats / minute, a blood pressure of 120/80 mmHg and a temperature of 37.3 ºC. The pleuro-plumonnary examination was in favor of a syndrome of fluid effusion. The chest x-ray revealed a right water tone opacity surmounted by a hydro-aerial level (figure 1).The thoracic CT revealed a right hydropneumothorax without parenchymal lesions or associated lymphadenopathies, the pleural puncture had objectified a exudative fluid with negative culture; Her blood cultures, cytobacteriological examination of sputum, her IDR and Koch's bacillus were negative. The patient did not have hypereosinophilia but the hydatid serology by ELISA was positive. There were no other cystic localizationsparticularly hepatics.

Figure 1: X-ray image of hydropneumothorax
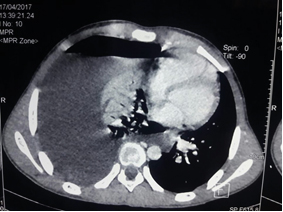
Figure 1.2: Chest scanner objectifying a hydropneumothorax
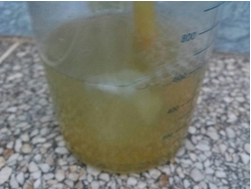
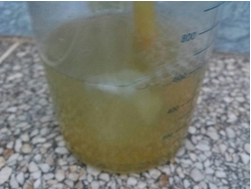
Figure 1.3: Image of hydatid membranes
The patient received surgical drainage with emission of false membranes through the chest tube, the parasitological analysis of which confirmed the hydatid nature of the cyst. In parallel with the drainage, the patient received a medical treatment based on albendazole for 6 months, the radiological evolution was progressively favorable with good aeration of the right lung.
Cystic echinococcosis is a human parasitic infestation that is caused by the larvae of the cestode Hydatid cysts preferentially involve the liver; however, any organ may be affected via the portal or systemic circulation. Cardiac ou pleural involvement is very rare even in endemic countries [2]. The usual locationsare the liver and lungs; intrathoracic but extrapulmonary locations like the pleura, diaphragm, mediastinum, pericardium,and chest wall are uncommon. Pleural hydatid cystscan develop chiefly as a result of liver or lung cyst ruptureinto the pleural space with complications of pneumothorax,pleural effusion, or empyema [3]. The clinical symptomatology is poor and nonspecific;it can simulate any pleural-pulmonary disease (chest pain,dyspnea, and dry cough). The diagnosis can be made in theacute phase in front of a symptomatology of sudden onset ofthoracic pain and dyspnea, following the rupture of the cyst. In other cases, this new location may remain asymptomaticfor a long time and the diagnosis can be done tardily. Exceptionally, there may exist some signs ofmediastinal compression depending on the location. The discovery can also befortuitous on a chest roentgenogram [4]. Imaging is a fundamental element for positive diagnosis. The chest roentgenogram shows a homogeneous pleural opacity, well-defined with water tonality. Rarely, it shows peripheral calcifications that it orientates the diagnosis. Ultrasound is a second-line examination; it is very efficient with a diagnostic specificity estimated at 96%. It can make the diagnosis and make the extension assessment and the surveillance. It can show multicystic or hydroaerial images when the hydatid cyst is broken. In many cases, it shows the proliferative membrane doubling inside the pericyst which is pathognomonic of hydatid cyst, confirms the liquid nature of pleural opacity, and evokes positive diagnosis especially in case of multivesicular form; it also makes it possible to detect a possible pleural effusion associated with it and to look for other cystic localizations, particularly abdominal ones. Computed tomography confirms the pleural localization of the well limited fluid mass unmodified by injection of the contrast product; it is more sensitive than the previous modalities and makes it possible to pose the diagnosis with a higher specificity and sensitivity. MRI provides diagnostic support in cases where cysts are not characteristic on ultrasound or CT, especially in pseudo-tumoral forms.Biologically, hypereosinophilia is generally absent in cases of intrathoracic hydatid disease [5], our patient the hydatidserologies was positive but the hydatid serologies are often negative in cysts isolated uncomplicated pleural The sensibility immunology increases significantly in case of complication or associated liver cyst [6]. The positive diagnosis is difficult to establish due to therarity of the condition and the lack of clinical, radiological, and biological specificity. Thediagnosis of certitude is almost always operative by visualizingthe hydatid membrane and/or daughter’s vesicles or afterpathological study of the operative piece in case of infected or thickened cyst [7]. The first approach should be chest drainage as soon aspleural effusion is accessible It helps to lift the emergency by evacuatingthe pleural effusion responsible for the noisy clinical picture ; This drainage allows driving alsoat positive diagnosis by showing membrane debris hydatid in the drainage fluid. Surgery remains the only cure. Heinvolves evacuating the cyst, treating the residual cavity and complications, and to privilege parenchymal conservative. The main actions taken are the cystectomies, pericystectomies, atypical parenchymal resections and sometimes lobectomies in combination with surgical treatment, medical treatment with antihelminthics (albendazol) helps prevent recurrence and get a cure hydatid cysts persisting in about 30% of cases at the daily dose of 10 to 15 mg / kg withappropriatefollow-up reevaluations [8].
The primary pleural localization of the hydatid cyst is very rare or even exceptional. Its discovery is often fortuitous. More rarely, primary pleural hydatid cyst is symptomaticwith a discreet and nonspecific clinical presentation. Imagingespecially in section, plays a fundamental role; it makes it possible to guide the diagnosis, to specify the topography and the relations with the neighboring organs, and to look for other localizations.The feature of our observation, compared to literature, is the clinical presentation, the absence of hypereosinophilia, the negative hydatid serology, and especially the diagnostic orientation thanks to imaging.
- N F Badji, B NDong, G Akpo, H Dème, M H Touré, et al. (2017) Apport de l’imagerie dans le diagnostic de kyste hydatique pleural primitif: à propos de deux cas. Mali Medical. 32:33–36.
- Turak O, Ozcan F, Sokmen E, Isleyen A, Okten R S, et al. (2014) Syncope as the primary manifestation of hydatid cyst. Herz.39:287–290. [Crossref]
- S J Kim, K H Jung, W Jo, Y S Kim, C Shin, and J H Kim ( 2011 ) A case of pleural hydatid cyst mimicking malignancy in a nonendemic country. Tuberculosis and Respiratory Diseases. 70:338–341.
- A Kumar, P Yadav, S Pahuja, and S Chaudhri (2016) Hydatid disease of pleura: a rare cause of recurrent pneumothorax. J of Case Reports. 273–276.
- S Gursoy, A Ucvet, H Tozum, A E Erbaycu, C Kul, et al. (2009) Primary intrathoracicextrapulmonary hydatid cysts. Texas Heart Institute J. 36:230–233. [Crossref]
- L Harzallah, M Bacha, A Garrouche (2007) Kyste hydatique pleural primitif : à propos d’une observation. Revue Medicale De Liege. 62:506–508.
- S J Kim, K H Jung, W Jo, Y S Kim, C Shin, et al. (2011) A case of pleural hydatid cyst mimicking malignancy in a nonendemiccountry. Tuberculosis and Respiratory Diseases. 70:338–341.
- Issoufou I , Harmouch H, Belliraj L, Ammor F, Rabiou S, et al. ( 2018) Management for hydatid cysts of the lung ruptured in the pleural cavity. Medecine et Santé Tropicales. 28:292-296.