India is considered as the capital of cardiometabolic conditions. Multiple studies have highlighted the early age of onset of Coronary Artery Disease (CAD) in the Indian population. Ethnicity and family history have been the primary drivers for this young age of onset that so far has been loosely defined as <45 years or as early as <35 years. We present a young normotensive Indian patient in visibly good health who came into the emergency room with chest pain. He was treated with primary angioplasty post diagnosis of Acute Inferior Wall myocardial infarction. This is the only case reported, from India, to our knowledge of a young 25- year old patient with CAD without any previous family history of CAD or any known risk factors. Increasing cardiovascular events especially in patients without family history such as ours indicates the need to institute population level screening programs and increase awareness of healthy lifestyle among the youth.
Prevention; Young Indian Asians; Coronary Artery Disease; Behavioral Risk; Age
Coronary Artery Disease (CAD) begins as a subclinical process, generally spanning several decades before eventually becoming symptomatic. There is, however, a substantial individual variability in terms of severity, rate of progression and age of onset. Multiple studies have shown that Indians have higher prevalence of CAD [1-2]. In addition to higher prevalence rates, it is also well established that Asian Indian individuals may develop CAD much earlier than their counterparts [2]. More than 50% of deaths in individuals below the age of 50 are related to cardiovascular diseases and around 25% of the Acute Myocardial Infarction (AMI) are contributed by patients less than the age of 45 [3-4].
Most commonly CAD in patients less than the age of 45 is termed as young CAD. It has been noted that the clinical presentation, risk profile, and coronary anatomy of young CAD patients differ from those of patients who develop CAD at an older age [1, 3 and 5]. For example, comparative analysis of young patients with STEMI and NSTEMI/ UA revealed that single-vessel disease was predominant in the STEMI group, whereas triple-vessel disease was predominant in the NSTEMI/UA group. In both groups, LAD was the most commonly involved coronary artery [6]. Dyslipidemia and hypertension showed statistically significant difference across two age groups (<45 and >45 years) [7].
Although a few studies have reduced the cutoff of young onset CAD to a lower age group, the prognosis and risk factors have remained relatively similar to what has been previously described [8-10]. Sinha et al has identified multiple risk factors that are statistically significantly different between the young age onset CAD and the not so young onset CAD including familial history of premature CAD [9]. The risk factors were seen to be as high as 25%, primarily genetic, in individuals below 35 years [10].
Healthy sons of individuals with CAD from both Indian and North European origin have shown higher risk profile for CAD indicating a propensity for faster onset of CAD [11]. Familial CAD while primarily considered to be genetic is an outcome of both genetic and non-genetic risk factors (e.g. smoking, physical inactivity, and poor dietary habits). For instance, a suboptimal diet was recently associated with about 65% of all cardiometabolic death in 25-45 year old individuals. Further, Micha et al have recently shown that CAD patients in a younger age group have a constellation of unhealthy behavioral habits [12]. While significant progress has been made, the cardiovascular event rates and mortality hasn’t significantly improved compared to those in the older patient group [8,13]. MAGNETIC study has been initiated to assess the profile of healthy members of the families of individuals who have had premature CAD [14].
The incidence of young CAD (i.e< 35years) has been reported to be around 1.2% to 2% but it’s very poorly studied and ill-defined in the Indian population except for a few studies who aimed to understand the risk factors and to create a prognosis approach [15,16]. A retrospective study of STEMI patients from India with an average age of 26 years has indicated that AMI in very young patients was highly prevalent in the urban population (63.9%). Even though 46.8% of the patients had a family history of premature CAD, behavioral risk factors (diet, smoking, etc) were equally prevalent [9].
A 10 year retrospective study was conducted which involved autopsies of 545 IHD cases including 95 young patients (<45 years of age) with the youngest patient being 18 years old. The prevalence was much higher than the population level data due to the enriched study group but gives unique insights into the characteristics of these young patients. Among these 95 patients, 84 patients had IHD related to atherosclerotic CAD. Interestingly, the known risk factors were found to be more in patients above 35 years compared to the ones below 30 years. Further, two patients each had hypertension and diabetes as the only known cardiovascular risk factors [17].
We present a case of a young individual (age 25) without a family history or known behavioral risk factors.
A 25 year old young male was rushed into the emergency department with severe chest pain and sweating. This was accompanied with nausea and abdominal discomfort. The patient indicated that the pain started around 5 AM in the morning and intensified with time and became unbearable around noon.
The patient was conscious, coherent and had no fever. The patient was normotensive with a blood pressure of 100/70 mmHg. He had a heart rate of 80 bpm. The patient’s lungs were also clear.
He declared himself to be a non-alcoholic and a non-smoker. He had no previous history of hypertension, diabetes or any other chronic metabolic or respiratory medical conditions. Additionally, the patient did not have any family history of CAD or other metabolic conditions.
The laboratory results indicated a normal CBC with hemoglobin levels (15 gm) and WBC of 10,000 cu.mm. He was negative for HIV I/II, HB1Cg, and HCV. Lipid profile showed serum cholesterol of 250 mg/dL, LDL of 140 mg/dl, HDL of 35 mg/dL, VLDL of 34 mg/dL, total triglycerides of 146 mg/dL RBS of 98 mg/dL, secretin of 0.9 mg/dL and blood urea of 32 mg/dL.He was Troponin 1 positive (210 pg/ L).
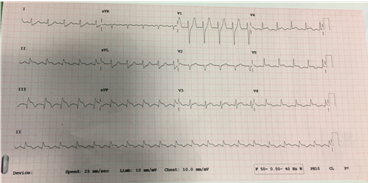
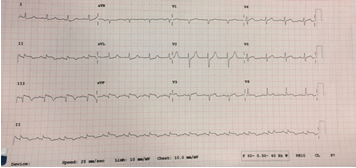
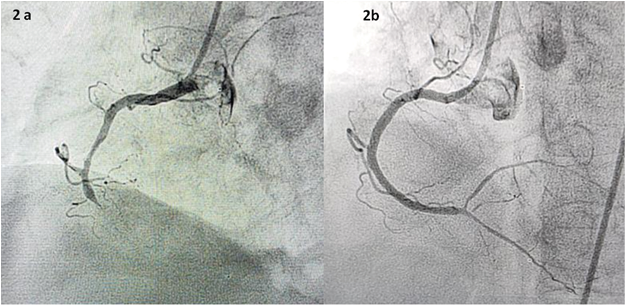
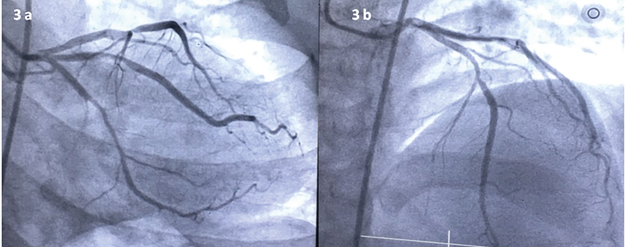
The electrocardiogram (ECG) showed an ST- Elevation in L2 L3 aVF, indicative of inferior wall STEMI (Figure 1a). The angiogram showed total occlusion of the right coronary artery (RCA) and an 80% block in the left anterior descending (LAD) coronary artery (Figure 2a and 3a). The patient was treated with primary angioplasty. Post- treatment ECGs showed ST- segment resolution (Figure 1b).
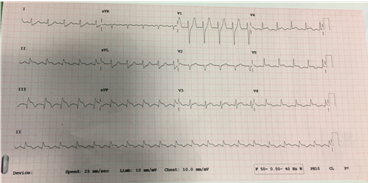
Figure 1(a): Electrocardiogram of the patient at admission showing ST elevation in L2 L3 aVF- indicative of Acute Inferior Wall MI.
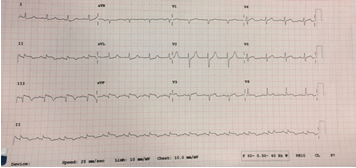
Figure 1 (b): Electrocardiogram of the patient post procedure showing ST segment near to resolution.
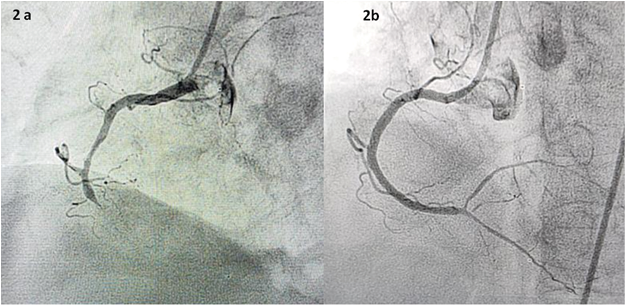
Figure 2: Angiogram of the RCA (a) with 100% occlusion and (b) clearance post procedure.
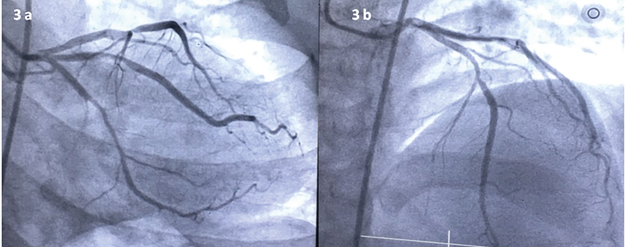
Figure 3: Angiogram of the LAD (a) with 80% lesion and (b) clearance post procedure.
The case of a young 25-year-old individual presenting with acute chest pain draws attention to the health status of the ill-understood strata of the Indian population. The patient did not have any family history of CAD nor did he have any of the known risk factors such as hypertension or obesity. He, also, declined being a smoker or an alcoholic.
India's impressive economic growth fueled by the alleviation of poverty accompanied by significant improvements in health outcomes especially in the communicable diseases is enviable by any nation. India is not only one of the fastest-growing economies of the world but it is also expected to become the third-largest economy by 2050. This is primarily because India is one of the youngest countries in the world with about 55% of the population below the age of 25.
However, the changing economic conditions are also having a significant impact on the lifestyle led by the young Indian population in urban as well as rural areas. While the increased incidence of chronic conditions specifically the cardiometabolic diseases have been highlighted in the younger Indian population, cases such as the one cited here draws our attention towards a. implications and impact on the youth (18 years to 30 years) and b. better understanding of both behavioral and genetic risk factors.
Last few decades have focused population level interventions for the “at risk” group especially in the hypertension and diabetes space. Recent studies have highlighted the impact of non-genetic factors and poor management of the same on the cardiometabolic burden especially in young adults [7,14]. A registry assessment from Canada highlighted that while cardiometabolic disease burden has reduced across many strata, the condition has not declined significantly in the young. This highlights the importance of increasing awareness and introducing proactive measures for at risk individuals [18]. With increasing enrollment of both unskilled and skilled workforce from an age group as young as 18 years with sparse yet alarming incidence of MI, IHD and stroke, population level understanding and interventions should include youth (18-30 years). Awareness around preventive healthcare measures that have profound impact on known risk factors, such as adoption of a healthy diet, abstinence from smoking and drinking, increased exercise etc., should be extended to these youth through newer digital methods for better adoption. Additionally all diagnostics offered both by the public and private sector should be availed by younger populations independent of their medical family history. Enrolling youth in awareness programs and implementing national health policies is no more an option but a necessity to ensure that young India becomes ‘Healthy India’ and delivers on the much promised economic growth.
- Badran HM, Elnoamany MF, Khalil TS and EzzEldin MM. Agerelated alteration of risk profile, inflammatory response, and angiographic findings in patients with acute coronary syndrome. Clin Med Cardiol. 2009;3:15-28. [Crossref]
- Sharma M andGanguly NK. Premature coronary artery disease in Indians and its associated risk factors. Vasc Health Risk Manag. 2005;1:217-25. [Crossref]
- Prajapati J, Joshi H, Sahoo S, Virpariya K, Parmar M and Shah K. Age related differences of novel atherosclerotic risk factors and angiographic profile among gujarati acute coronary syndrome patients. J Clin Diagn Res. 2015; 9(6):OC05-9. [Crossref]
- Prabhakaran D, Jeemon P, and Ambuj Roy. Cardiovascular diseases in india current epidemiology and future directions. Circulation. 2016;133:1605-1620. [Crossref]
- Yildirim N, Arat N, Doğan MS, Sökmen Y and Ozcan F. Comparison of traditional risk factors, natural history and angiographic findings between coronary heart disease patients with age <40 and >or=40 years old. Anadolu Kardiyol Derg. 2007; 7:124-7. [Crossref]
- Deora S, Kumar T, Ramalingam R and Manjunath CN. Demographic and angiographic profile in premature cases of acute coronary syndrome: analysis of 820 young patients from South India. Cardiovasc Diagn Ther. 2016;6(3):193-198. [Crossref]
- Adam AM, Rehan A, Iqbal U, Saleem H, Ali MA, Shaikh A, et al. Prevalence of conventional risk factors and evaluation of baseline indices. J Clin Diagn Res. 2017;11(7):OC34-OC39. [Crossref]
- Aggarwal A, Srivastava S, Velmurugan M. Newer perspectives of coronary artery disease in young. World J Cardiol. 2016;8(12):728-734 . [Crossref]
- Sinha SK, Krishna V, Thakur R, Kumar A, Mishra V, Jha MJ, et al. Acute myocardial infarction in very young adults: A clinical presentation, risk factors, hospital outcome index, and their angiographic characteristics in North India-AMIYA Study. ARYA Atheoscler. 2017;13(2):79-87. [Crossref]
- Lakshmy R, Dorairaj P, Tarik M, Gupta R, Reddy KS. LDL particle heterogeneity, and its association with other established cardiovascular risk factors in a young Indian industrial population. Heart Asia. 2012:141-145. [Crossref]
- Shaukat N, de Bono DP, Jones DR. Like father like son? Sons of patients of European or Indian origin with coronary artery disease reflect their parents' risk factor patterns. Br Heart J. 1995;74:318-323. [Crossref]
- Micha R, Penalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarin D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017; 317(9):912–24. [Crossref]
- Garshik M, Vaidean GD, Vani A, Underberg JA, Newman JD, Berger JS, et al. Cardiovascular Risk Factor Control and Lifestyle Factors in Young to Middle-Aged Adults with Newly Diagnosed Obstructive Coronary Artery Disease. Cardiology. 2019;142(2): 83-90. [Crossref]
- Osadnik T, Osadnik K, Pawlas N, Strzelczyk J, Kasperczyk J, Polonski L, et al. Metabolic and genetic profiling of young adults with and without a family history of premature coronary heart disease (MAGNETIC). Study design and methodology. Arch Med Sci. 2019;15 (3):590-597. [Crossref]
- Dattatrya K, Vedpalsingh TH , Goraknath WV, Kiran PS. Can erectile dysfunction in young patients serve as a surrogate marker for coronary artery disease?. J Clin Diagn Res. 2015;9(11): PC01-PC03. [Crossref]
- Dalal J, Hiremath MS, Das MK, Desai DM, Chopra VK, Biswas AD. Vascular disease in young indians (20-40 years): role of ischemic heart disease. J Clin Diagn Res. 2016;10(9): OE08-OE12. [Crossref]
- Vaideeswar P, Tyagi S, Singaravel S. Pathology of atherosclerotic coronary artery disease in the young Indian population. Forensic Sci Res. 2019;4: 241-246. [Crossref]
- Vikulova D, Grubisic M, Zhao Y, Lynch K, Humphries KH, Pimstone SN, Brunham LR. Premature atherosclerotic cardiovascular disease: trends in incidence, risk factors, and sex-related differences, 2000 to 2016. J Am Heart Assoc. 2019;8(14):e012178. [Crossref]