The ECG interpretation in severe acidosis is difficult. It is thought that acidosis alters the myocyte cell membrane permeability leading to electrolyte shifts across the membrane. Correcting it by bicarbonate administration to patients with severe metabolic acidosis remains controversial especially in diabetic ketoacidosis as it is recommended to give bicarbonate only in case of associated renal insufficiency [1, 2]
Diabetic Ketoacidosis; Acute Coronary Syndrome; Electrocardiography; Acidosis; Sodium Bicarbonate
Diabetes mellitus is a prevalent disease accounting for many complications; one of the most devastating is DKA following alterations in glucose metabolism caused by infection, injury or myocardial infarction. Early recognition and treatment are required to prevent further damage.
Metabolic acidosis results either from loss of bicarbonate from the body e.g. diarrhea or from its titration to an anionic base that often can be converted back to bicarbonate like in diabetic acidosis or lactic acidosis. This anionic base is commonly named “potential” bicarbonate. Giving bicarbonate in patient with a true bicarbonate deficit is not controversial. Argument rises when the decrease in bicarbonate concentration is the result of its conversion to another base which by time can be converted back to bicarbonate.
Severe acidosis causes a reduction in myocardial contractility, a fall in cardiac output, and a fall in BP as it slows the intraventricular conduction. Acidemia reduces the binding of norepinephrine to its receptors. It also shifts the oxyhemoglobin curve to the right, allowing more O2 to be released (The Bohr Effect). A Proton H+ binds to intracellular proteins and extracellular proteins, especially albumin and haemoglobin. Thus, Acidemia may adversely affect cell functions such as enzymatic reactions, ATP generation and fatty acid biosynthesis [3, 4]. On the other hand, Bicarbonate therapy is also associated with an increase in mortality. This has been noted in humans and experimental animals under a variety of acidosis conditions [5, 6].
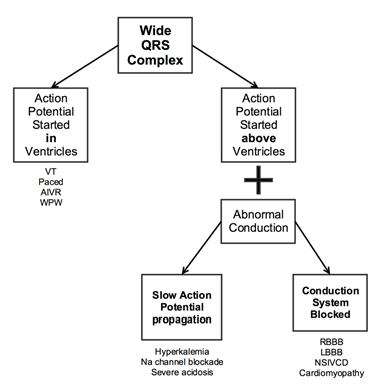
In general, bicarbonate should be given at an arterial blood pH of ≤7.0. The amount given should be what is calculated to bring the pH up to 7.2. The use of bicarbonate in treating wide QRS complex is well-known only in the setting of antidepressant toxicity by reversing drug-induced sodium channel blockade.
We demonstrate in this case that giving bicarbonate remains a useful approach in order to provide the needed treatment in the setting of late stage DKA and wide QRS complex without antidepressant toxicity.
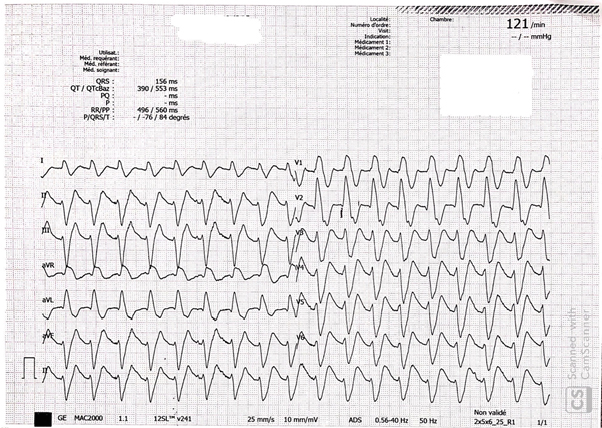
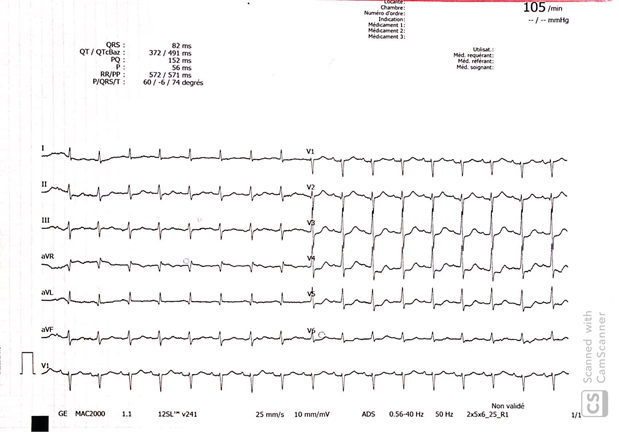
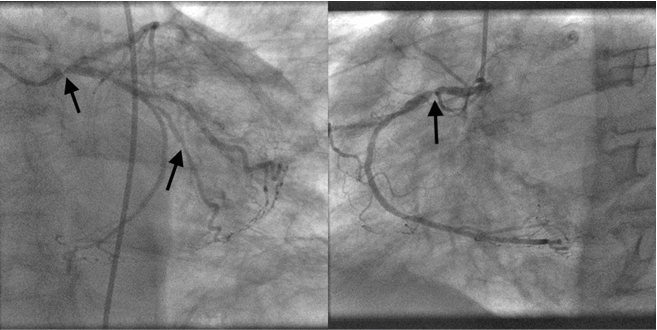
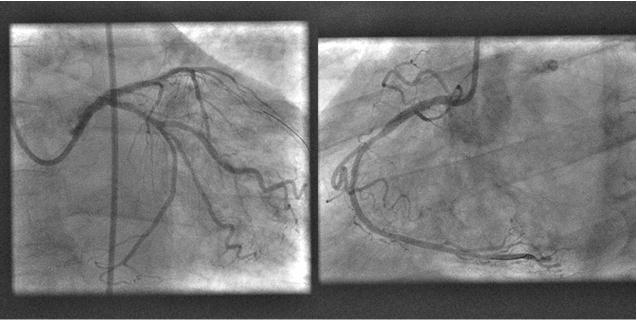
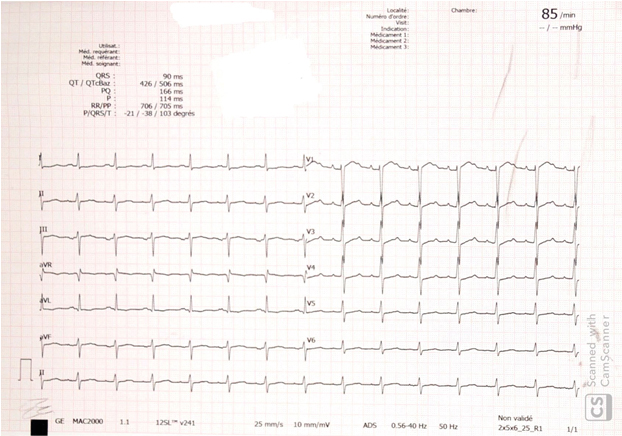
A 75-year-old male known to have Alzheimer’s disease and long-standing insulin-dependent diabetes mellitus. Present to our emergency room for three days history of altered general status, nausea and vomiting. Family state that the patient complains of a sub sternal progressive chest pain. Vital signs at presentation showed a blood pressure of 113/65 mmHg, heart rate of 98 bpm, tachypnea at 37/min. ABG showed: pH 6.9 (N 7.35-7.45), PO2 80 mmHg (N 65-105), PaCO2 19 mmHg (N 35-45), low bicarbonates 17 mEq/l (N 22-26 mEq/l), lactates 12 mmol/l. Other blood lab tests: elevated fasting blood glucose 480 mg/dl (N 72 to 99 mg/dl), normal potassium level at 3.9 mmol/l (N 3.5-5.0), elevated high sensitivity troponins at 642 ng/l, Pro BNP 2500 pg/ml, hemoglobin 12 g/dl, hepatic and renal functions were within normal limits, urine ketones were positive. The first ECG revealed large QRS complexes with a ventricular rate of 121, no ST-segment changes could be appreciated Figure 1, which is not related to potassium level changes. The diagnosis of late stage diabetic ketoacidosis was established and the patient was started on intravenous fluids and insulin. Intravenous sodium bicarbonate was also given and ECG was repeated few hours later which showed a normalization of QRS complex width, ST-segment elevation in the aVR > 2 mm, and ST depression in V3 to V6 and inferior leads. Figure 2 Transthoracic echocardiogram showed anterior, septum, apex, and inferior wall hypokinesia. The patient was taken to the Cath lab where coronary angiography showed 3-vessel disease with subtotal occlusion of left main coronary artery, second marginal and proximal right coronary artery. Figure 3 Left main and proximal right coronary arteries were stented successively with good results. Figure 4 The subsequent ECG showed complete ST segment resolution. Figure 5
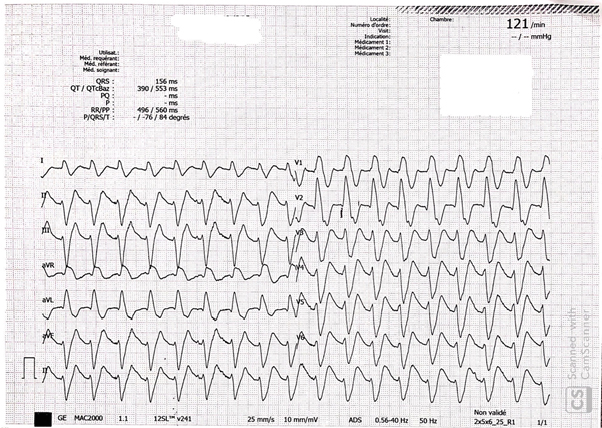
Figure 1: The First ECG Revealing Large QRS Complexes with a Ventricular Rate of 121, No ST-Segment Changes Could be Appreciated.
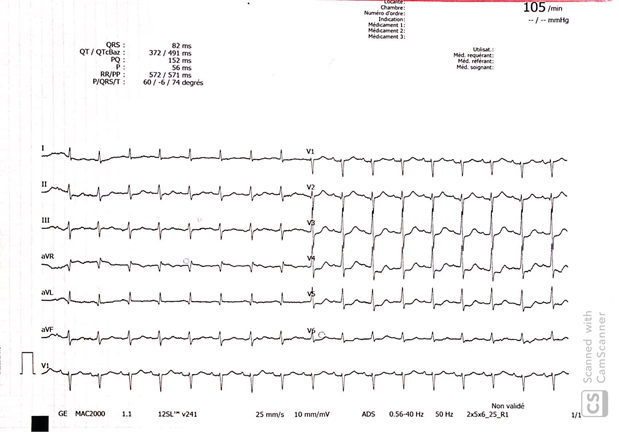
Figure 2: Normalization of QRS Complex Width And Unveiling An ST-Segment Elevation In Avr > 2 Mm And ST Depression In V3 To V6 And Inferior Leads.
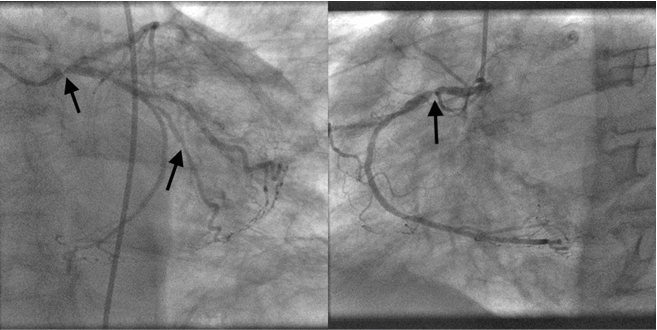
Figure 3: Severe Stenosis of Left Main Coronary Artery, Second Marginal and Proximal Right Coronary Artery
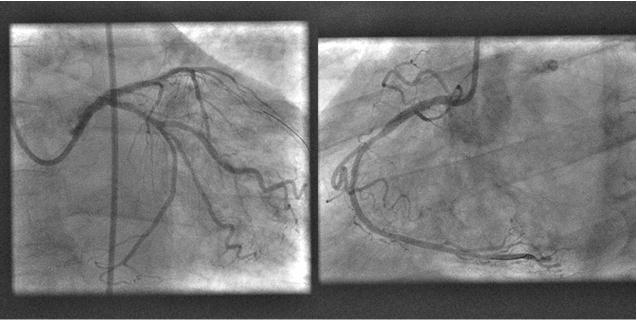
Figure 4: Left Main and Proximal Right Coronary Arteries Were Stented Successively With Good Results
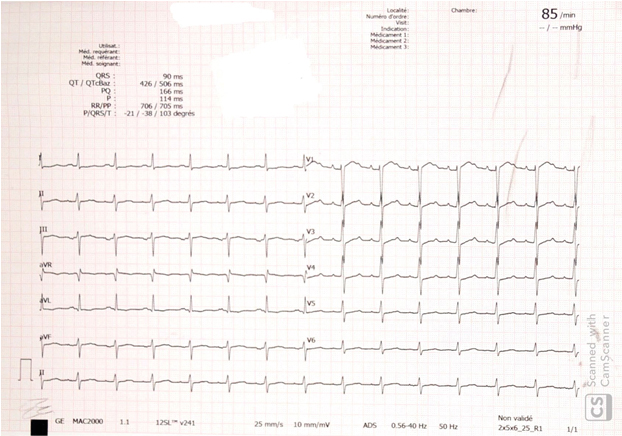
Figure 5: Complete ST Segment Resolution
The specific ECG changes of severe acidosis are challenging. B y searching PubMed and Google Scholar, varying ECG changes in patients with DKA were described in literature mostly related to hyperkalemia such as ST-segment elevation or depression, tall T waves, U waves and widening QRS [7] complicating its relevance in cases of severe late stage acidosis with normokalaemia.
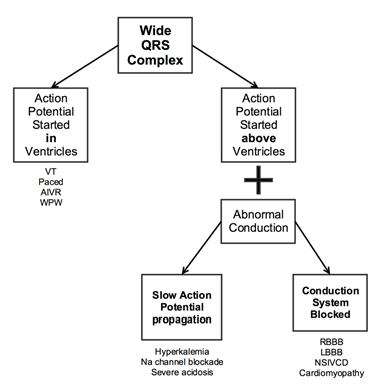
Pseudo-infarction is a term used in literature referring to ECG resembling infarction with normal myocardium in patients with DKA [8] whereas true myocardial infarctions mostly affect the conduction system i.e. LBBB, RBBB, AV block, or NSIVCD [9]. This case highlights the potential masking effect of severe acidosis by slowing the action potential propagation at the level of myocytes as well as prolonging QTc that occurs frequently during DKA and its correlation with acidosis [10] making it challenging per se to determine if there is underlying ischemic changes. Table 1 The degree of this effect differs depending on the amount and duration of acidosis and tends to resolve with the resolution of acidosis in addition to an increased mortality rate to the degree of acidosis [11].
Table 1. Algorithm for Determining Conduction Anomaly
Limiting the use of Bicarbonates in diabetic ketoacidosis for renal insufficiency only is debatable as its impact on regressing the QRS widening in acidosis is vital as demonstrated in this case. Troponins alone are not specific in DKA as high levels appear without acute coronary syndrome [12]. Therefore, Bicarbonates administration with carful usage would be a helpful way to ascertain any undermined anomalies by unmasking hidden ECG changes among patients with no clear symptoms either due to altered mental status or diabetic neuropathy and painless myocardial infarction.
Finally, severe acidosis in DKA could hide ischemic ECG changes, as well as producing a vicious circle that is the infarction leading to acidosis and acidosis altering cardiac cellular function [13] hence rapid correction is needed.
Early detection of any underlying anomaly is critical for successful management. As illustrated in our case, severe acidosis in DKA with normokalaemia should be considered as an independent factor causing conduction abnormalities and masking ischemic changes on ECG especially in the absence of symptoms in hypoalgesia or cognitive impairment.
- Okuda Y, Androgue HJ, Field JB, et al. (2000) Counterproductive effects of sodium bicarbonate in diabetic ketoacidosis. J Clin Endocrinal Metab 81: 314-319. [Crossref]
- Makiasalo JH, Soini HO, Nordin HJ (1989) Effects of bicarbonate therapy on tissue oxygenation during resuscitation of hemorrhagic shock. Crit Care Med 17: 1170-1174. [Crossref]
- Luft F (2001) Lactic acidosis update for critical care clinicians. J Am Soc Nephrol 17: S15-S19. [Crossref]
- Androgue HJ (2006) Metabolic acidosis: Pathophysiology diagnosis and management J Nephrol 19: S62-S69. [Crossref]
- Sing RF, Branas CA, Sing RF (1995) Bicarbonate therapy in the treatment of lactic acidosis: Medicine or toxin? J Am Osteopath Assoc 95: 52-57. [Crossref]
- Gehlbach BK, Schmidt GA (2004) Bench-to-bedside review: Treating acid-base abnormalities in the intensive care unit-The role of buffers. Crit Care 2004 8: 259-265. [Crossref]
- Kenneth LD, Ron MW (1986) Hyperkalemia: ECG manifestations and clinical considerations. J Emerg Med 4: 449-455. [Crossref]
- Rahat AT, Anna S, Mark E (2018) Diabetic ketoacidosis and myocardial 'pseudo infarction'. Endocrine Abstracts 56: EP77. [Crossref]
- Gorenek B, Lundqvist CB, Terradellas JB, et al. (2014) Cardiac arrhythmias in acute coronary syndromes: position paper from the joint EHRA, ACCA, and EAPCI task force. Eur Heart J Acute Cardiovasc Care 4: 386-386. [Crossref]
- Omneya I Youssef, Samar M Farid (2012) QTc and QTd in Children with Type 1 Diabetes Mellitus during Diabetic Ketoacidosis. International Scholarly Research Network ISRN Pediatrics. [Crossref]
- Allyn J, Vandroux D, Jabot J, et al (2016) Prognosis of patients presenting extreme acidosis (pH <7.0) on admission to intensive care. J Crit Care 31: 243-248. [Crossref]
- Demet MG, et al. (2016) Markedly Elevated Troponin in Diabetic Ketoacidosis without Acute Coronary Syndrome. Turk J Endocrinol Metab 20:58-60. [Crossref]
- MA Neaverson (2016) Metabolic Acidosis in Acute Myocardial Infarction. BMJ 2: 383-385. [Crossref]