Hypnotherapeutic interventions for psychological support in stressful situations show promising effects in many areas. This case report discusses some of the results of a feasibility pilot study of brief psycho-oncological interventions during cancer treatment, focusing on the effects of self-hypnosis. Despite some methodological limitations of the study, there is evidence that self-hypnosis interventions may have lasting impacts on strengthening coping skills.
Coping with Cancer; Emotional Distress; Self-Hypnosis; Resource Activation; Brief Interventions in Psycho-Oncology
The most common feelings that individuals with cancer suffer from are emotional distress, anxiety, fear of progression or relapse, and depressive moods. These subsyndromal symptoms occur in over 50% of oncological patients [1]. The severity of emotional distress can range from “normal” feelings of vulnerability or sadness to episodes of major depression and anxiety disorders [2]. Side effects and physical symptoms such as nausea, loss of appetite and digestive problems, pain, sleep disorders, cognitive impairment, and the symptom complex of weakness and exhaustion are particularly present during oncological therapy. The therapeutic context is sometimes experienced as a "problem trance," with narrowed, focused attention to threatening issues, persistently circling thoughts, loss of control, and a cognitive dissociation from helpful resources. Hypnotherapeutic interventions have been shown to provide beneficial results in coping with these stresses [3-5]. However, there is still a need to clarify how short interventions with a few sessions can be integrated into oncological therapy.
To better support individuals with cancer and enhance coping skills, we have developed a short psycho-oncological program (HypRa) based on resource activation [6-7] to accompany clinical therapy and tested its feasibility [8].
The HypRa (Hypnosystemic Resource activation) pilot study program, a unique offering of brief Cognitive Behavioral Interventions (CBI) or Hypnotherapeutic Interventions (HTI), was specifically tailored for individuals with cancer undergoing chemotherapy or immunotherapy. The program was conducted at the oncology outpatient clinics of the Ulm University Hospital.
HypRa was positioned to help clients find perspectives on well-being and solutions to cope with stress by activating their abilities. Of the approximately 200 individuals who were offered participation in the study, 34% expressed interest in taking part. The sample of N=60 participants who completed the study was distributed as follows: 13 male (22%), 47 female (78%); mean age 55.87 years (SD=10.83); oncological diseases: breast or gynecological 27 (45%), gastrointestinal 18 (30%), other 15 (25%); mean duration of disease was 21.88 month, ranging from 1 month to 243 months (SD 42.09, median=8 months); initial diagnosis 38 (63%), recurrence 22 (37%).
Participants were assigned to the two intervention groups—CBI or HTI—based on their available time windows. Importantly, this assignment was irrespective of the oncological diagnosis and duration of illness. Individuals who expressed interest in the study but could not participate in the interventions during the first recruitment phase were assigned to a waiting control group with the opportunity to join the program later. In the meantime, they received CAU (care-as-usual).
Compared with established cognitive behavioral interventions, the pilot study focused on the applicability of brief hypnotherapeutic interventions, particularly self-hypnosis. The interventions consisted of three individual one-hour sessions every two weeks.
Both interventions, HTI and CBI, started with psychoeducation to explain the psychophysiological mechanisms of individual stress experiences, encouraging participants to modulate these mechanisms by activating personal resources [9, 10]. The cognitive behavioral intervention (CBI) then focused on methods based on mindfulness, self-care, and communication skills. These methods are considered the 'gold standard' in supportive psycho-oncological treatment associated with emotional relief and stabilization, better coping with cancer distress, and enhanced quality of life [11, 12].
The hypnotherapeutic intervention (HTI) began with an introduction to a first trance experience, e.g., a journey to a personal “place of well-being” combined with a guided imagination promoting beneficial emotional experiences with a “representative technique” [13]. The representative figures metaphorically symbolize resources such as power, release, safety, trust, hope, and clarity and allow individuals more straightforward access to their emotional resources. Participants were asked to continue practicing the trance experience as self-hypnosis using a pre-recorded take-home audio file containing imaginations about well-being, safety, trust, and hope. In the second session, an individual trance story was developed and recorded with the participant for further practice at home. In the third session, the self-hypnosis experiences were evaluated and, if necessary, modified for further individual coping with stress. Finally, patients were encouraged to practice self-hypnosis in stressful situations, as a tool available at any time, in any place, independent of the presence of a hypnotist. For example, patients can hypnotize themselves in the operating room, during radiotherapy, in an infusion suite, in a hospital bed, or at night if they are having trouble falling asleep [5].
In both intervention groups, participants received homework to reflect on personal resources, strengths, and skills for coping with stress and crises. The reflection ideas were discussed at the beginning of the second and third sessions. At the end of the final session, the reported experiences and findings during the interventions were summarized, and participants were informed that another questionnaire would be sent approximately three months after this session.
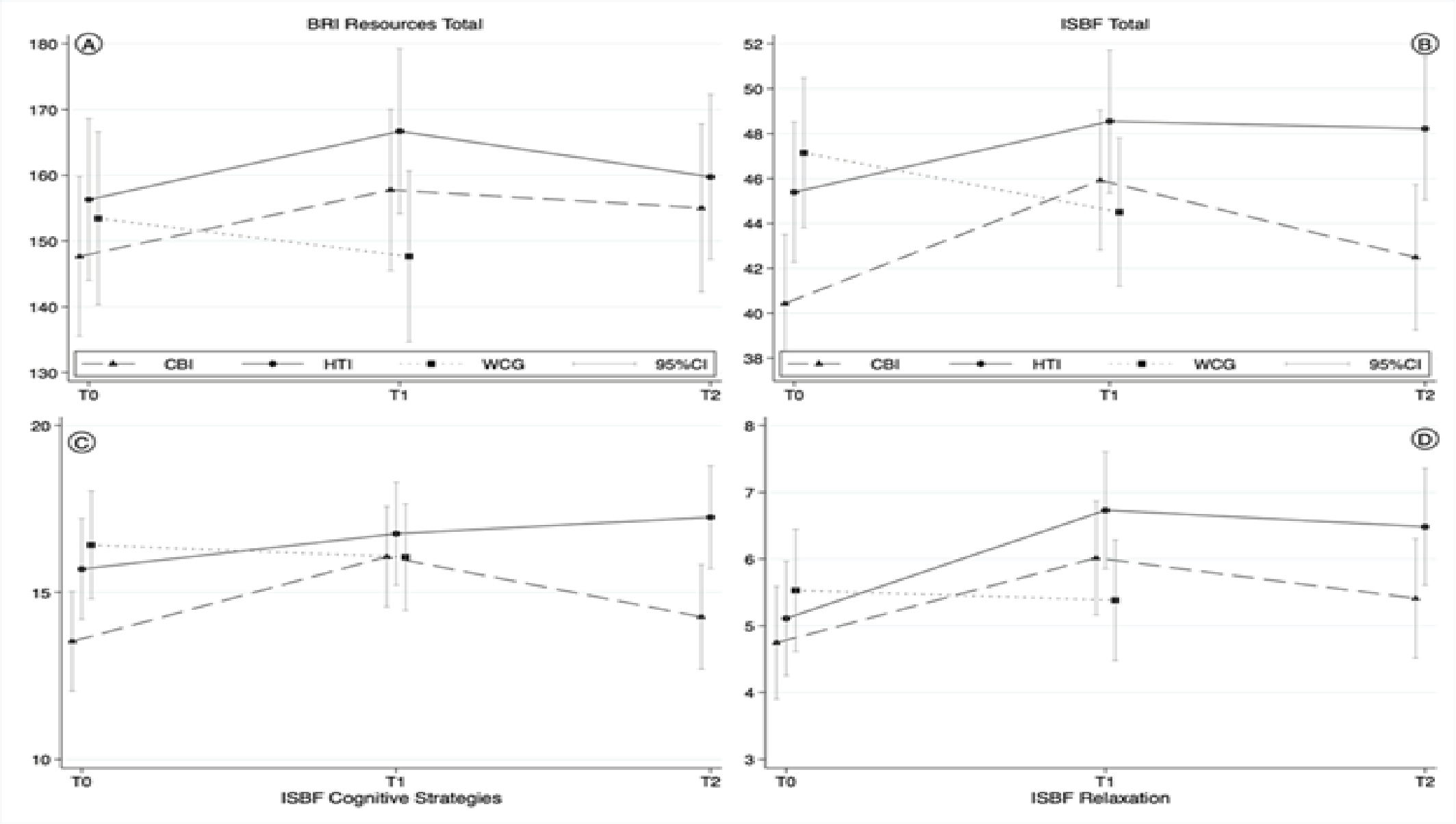
Resource activation and stress management capabilities were measured using standardized questionnaires. The Bern Resource Inventory (BRI) assesses a certain level of activating personal resources [14]. The Inventory of Perceived Stress Management Skills (ISBF) measures personal stress management abilities, covering cognitive strategies, use of social support, relaxation strategies, anger regulation, and perception of bodily tension [15]. Changes were examined at three measurement points (T0: baseline, T1: 1 month after treatment, T2: 3 months follow-up). Multilevel linear regression models with mixed effects were used and adjusted for diagnosis and duration of illness since initial diagnosis. Preliminary results, interpreted with great caution, support the effectiveness of both methods, while self-hypnosis appears to have a longer-lasting effect.
Concerning activating their resources, both groups showed higher scores at T1 compared to T0 (p ≤ 0.05), measured by the BRI (see contrasts in Table 1). The total score for stress management skills as measured by ISBF increased for both groups from T0 to T1 (p ≤ 0.001 for CBI, p ≤ 0.01 for HTI). The score for CBI returned almost to baseline (p ≤ 0.01), while the increase for HTI persisted at T2(p ≤ 0.05). For CBI, the stress management subscore on cognitive strategies increased from T0 to T1 (p ≤ 0.001) and decreased again at T2 (p ≤ 0.01), while the score for HTI increased continuously from T0 to T2 (p ≤ 0.01). The stress management subscore for relaxation skills increased at T1 for CBI and HTI (p ≤ 0.001). For HTI, this score increased significantly from T0 to T2 (p ≤ 0.001). For WCG, there were no significant changes from T0 to T1 (see Table 1).
Table 1: Contrasts within predictors
Variables |
Comparison within HTI |
Comparison within CBI |
|
T1 vs T0 |
T2 vs T0 |
T2 vs T1 |
T1 vs T0 |
T2 vsT0 |
T2 vs T1 |
BRI Resources Total |
10.36* |
3.73 |
-6.62 |
10.15* |
6.97 |
-3.18 |
ISBF Total |
3.12** |
3.00* |
-0.12 |
5.52*** |
1.68 |
-3.84** |
ISBF Cognitive Strategies |
1.06 |
1.56** |
0.50 |
2.54*** |
0.72 |
-1.82** |
ISBF Relaxation |
1.62*** |
1.39*** |
-0.23 |
1.27*** |
0.63 |
-0.64 |
*p < 0.05; **p < 0.01; ***p < 0.001
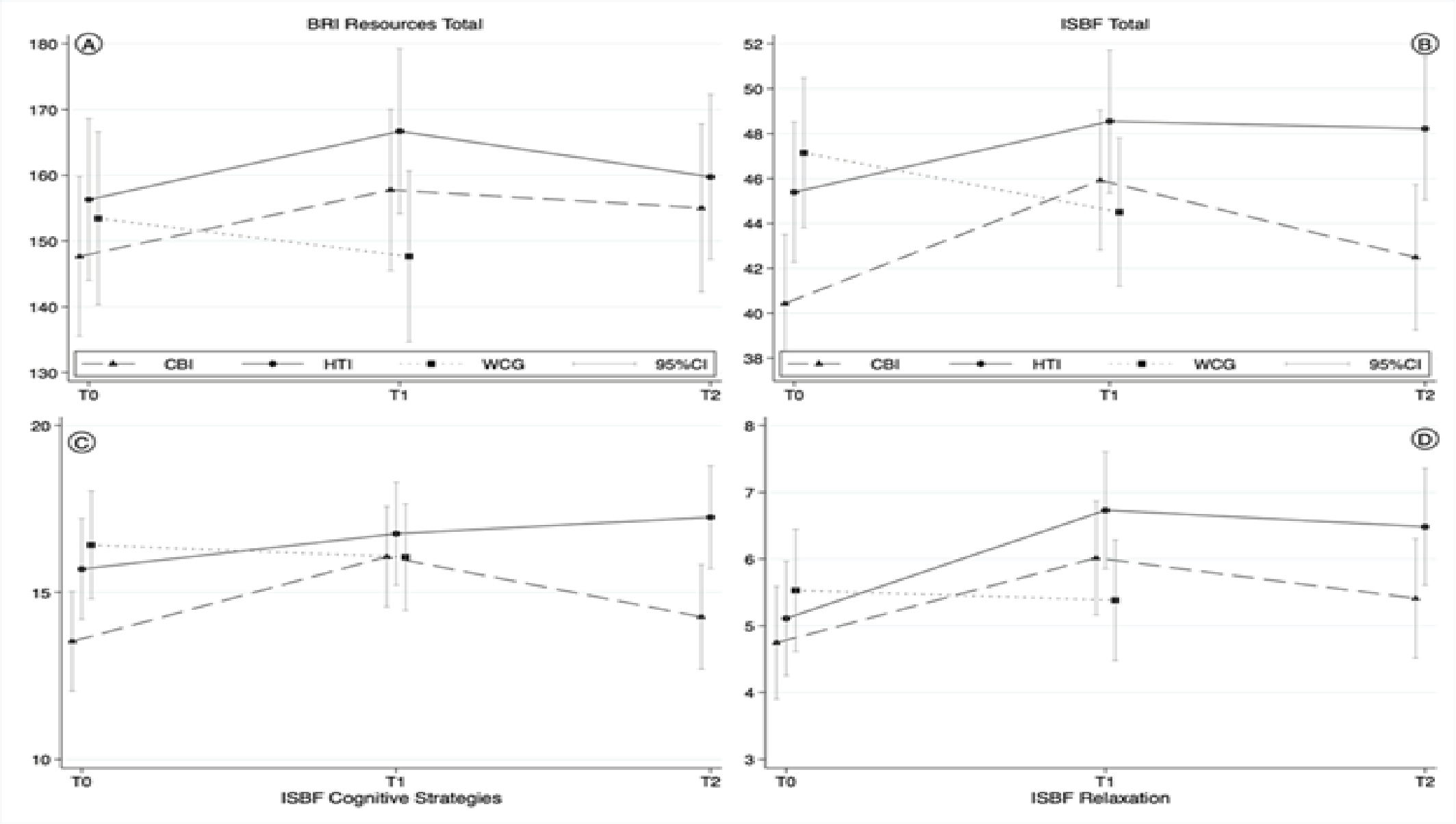
Figure 1: Results from linear mixed-effects regression models for resources and stress management skills
A) BRI Resources (Total Score), B) ISBF (Inventory for Stress Management Skills) total score, C) ISBF Cognitive Strategies, and D) ISBF Relaxation Techniques. Models were adjusted for diagnosis and duration of disease. Models were adjusted for diagnosis and duration of disease. For ethical reasons, there was no catamnesis in the WCG participants, especially since there were no changes between the measurement times T0 and T1. If interested, these individuals should be able to participate in the intervention program offered as soon as possible.
When interpreting the results, it is crucial to acknowledge the limitations of the study design, including the small number of participants and incomplete randomization. These constraints necessitate a cautious discussion of the findings' implications, but they may guide future investigations.
After three individual sessions, the CBI and HTI groups significantly improved stress management and emotional well-being, surpassing the WCG. In particular, the self-hypnosis intervention appeared to have lasting effects on stress management skills, including cognitive strategies, problem-solving abilities, and relaxation techniques. The lasting effect of the self-hypnosis intervention can also be interpreted as mental prophylaxis for dealing with possible future crises.
This remarkable aspect raises an interesting question: What factors make self-hypnosis a practical complementary therapy approach? At its core, hypnotherapy is a resource-based approach that helps increase self-efficacy by promoting a sense of control and resilience by discovering individual solutions and problem-solving strategies. While the level of impairment and suffering from the burden of disease may vary over time, emotional vulnerability, sometimes with critical escalations, often persists [16]. So, individuals may also be more susceptible to negative or positive suggestions. In this context, hypnotherapeutic interventions seem to be ideally suited to freeing patients from this "problem trance" and enabling a positive change of perspective. They are relatively easy and inexpensive to provide, have a plethora of beneficial "side effects" (such as an increased sense of control over pain and its impact and an increased sense of well-being), and have very few adverse side effects [17] .
Hypnotherapeutic interventions can utilize the client's imagination to induce a resource-activating trance state through calming visual journeys or mental images. These procedures are non-invasive and deeply relaxing. They enhance the client's capacity to respond to suggestions without physical effort [18, 19].
Even individuals with severe illness can benefit from these interventions. They help with the physical and emotional representation of experiences that arise through imaginative work in a trance, providing access to resource experiences lost during illness and treatment. For many cancer patients, their bodies have become alien throughout the disease, usually just a source of discomfort and pain. However, the (re)activation of an experience of physical well-being through imagination in a trance can change this perception. It allows the patient to realize that such a physical experience is still possible, regardless of the discomfort. This realization often has a motivating effect and allows hope to grow.
Moreover, hypnotherapy plays a crucial role in cognitive work, ensuring an embodied anchoring (consolidation) of the therapeutic content. The activation and consolidation of the work done in self-hypnosis in the sense of such an embodiment contribute significantly to the change processes being able to take effect more quickly, holistically, and often more sustainably. This aspect of hypnotherapy is particularly beneficial, making it a valuable addition to behavioral therapy and psychodynamic working methods [4].
We were encouraged to take this approach as many studies already report positive effects in the hypnotherapeutic treatment of symptoms in cancer patients [3-5]. These studies typically focus on distress associated with medical procedures [20], nausea and vomiting [21, 22], hot flashes [23], and pain [24-26]. According to the results, there are some indications that just a few hypnotherapeutic sessions are enough to bring about lasting relief from physical symptoms.
One fascinating area of research is the investigation of the effectiveness of short interventions, such as those consisting of only three sessions, in a clinical setting and comparison to other approaches as a relatively new area of research [27-30], and the potential findings could significantly advance our understanding of the role of hypnotherapy in cancer treatment.
The hypnotherapeutic approach of the HypRa program harnesses individually significant resources, reactivating them to instill feelings of strength, hope, or comfort in the patient. These resources, unique to each individual, are identified, applied, and trained through self-hypnosis.
The effectiveness of self-hypnosis has been extensively documented in various clinical areas and is even considered a 'first-line' treatment for many chronic health conditions [17, 31, 32]. What sets self-hypnosis apart is its practicality in everyday situations, such as sports [33, 34], making it a low-threshold and relatively easy method. It empowers the client with a sense of self-control, a crucial aspect, especially for oncology patients. Another advantage is its flexibility, as it can be practiced outside the clinical environment, for instance, at home. However, for lasting effectiveness in a clinical context, the procedure must be taught and learned under the guidance of an experienced therapist [35].
The learning process is a crucial aspect to highlight here. It could also explain the possible sustained positive catamnesis effect for the hypnotherapeutic group in this study. According to Diamond and Frankel, hypnosis is a 'learnable coping style'. To elaborate, the authors suggest that elements such as patient preparation, demystification of hypnosis, attitudinal factors, an excellent therapeutic context, and the teaching of cognitive strategies to enhance hypnosis can all contribute to a patient's ability to learn hypnosis, even if they don't initially possess imaginative solid skills. This implies that someone's susceptibility to hypnosis is likely a learned coping style [36, 37].
Cognitive-behavioral approaches, including psychoeducational methods, are widely used and well-established in psycho-oncology. Some studies have already designed combined cognitive behavioral and mindfulness approaches with hypnotherapeutic interventions in psycho-oncology settings. The results are promising and underline our recommendation for a combination, as hypnosis and mindfulness seem to enhance the efficacy and benefits of other therapeutic approaches [38-42].
Eason (2013) argues that (many) hypnotherapists also incorporate hypnosis into other well-established psychotherapeutic interventions. “The same can be said about how we apply self-hypnosis. For example, hypnosis goes well with cognitive behavioral therapy (CBT) because many of the processes and techniques used in cognitive behavioral therapy (the mental imagery techniques) have real parallels to those used in hypnosis and self-hypnosis … The results of the Kirsch et al. (1995) meta-analyses of 18 studies that compared CBT with and without hypnosis as an adjunct found fairly significant improvements when hypnosis was used as an adjunct to the treatment [39]. (So) it seems to make sense that we can therefore employ a number of strategies from the field of CBT within our self-hypnosis sessions” [43]. Grégoire et al. (2020) found that an intervention combining self-care and self-hypnosis improved cancer patients’ self-esteem, emotional distress, emotion regulation strategies, and mindfulness abilities. Self-hypnosis was seen as a facilitator for these changes [44].
In a pilot study, the feasibility of integrating a short psycho-oncological program called “HypRa” into the outpatient care of cancer patients was tested. This case report discusses the potential benefits of the program, with particular emphasis on self-hypnosis. Although the methodology had some limitations, there is promising evidence that cognitive behavioral therapy with mindfulness or self-hypnosis can improve coping skills after three sessions. Additionally, self-hypnosis interventions could have lasting effects. Based on the resource activation principle described in this report, we suggest a brief intervention approach that combines cognitive-behavioral self-care, mindfulness, and hypnotherapeutic interventions to develop the HypRa program further. We recommend investigating this approach in a larger randomized controlled trial.
We thank Prof. Hartmut Döhner, the director of the Clinic for Internal Medicine III, University Ulm Medical Center; Prof. Wolfgang Janni, the director of the Clinic for Gynecology and Obstetrics, University Medical Center; Dr. Regine Mayer-Steinacker, Senior physician and coordinator at the Comprehensive Cancer Center Ulm; Prof. Jens Huober, director of the Breast Center at the Cantonal Hospital St. Gallen; Daniela Bodschwinna, Magdalena Wanner, and Madeleine Volz of the Department of Psychosomatic Medicine and Psychotherapy, University Ulm Medical Center, and the medical and nursing teams at the Outpatient Clinics of the University Ulm Medical Center Ulm for their support in conducting the feasibility study. We thank the German Society for Hypnosis (DGH) and the Comprehensive Cancer Center Ulm for financial support.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
The protocol of the study was approved by the Institutional Review Board of Ulm University (No. 431/16, 08/02/2017) and registered at the German Trials Register (DRKS00019095). The study complied with the Declaration of Helsinki, the Guideline for Good Clinical Practice, and local regulatory requirements.
- A. Mehnert (2018) One in two cancer patients is significantly distressed: Prevalence and indicators of distress. Psychooncology 27: 75-82. [Crossref]
- L. E. Carlson (2017) Distress Management Through Mind-Body Therapies in Oncology. JNCI Monogr 52. [Crossref]
- L. E. Carlson (2018) The Role of Hypnosis in Cancer Care. Curr. Oncol. Rep 20. [Crossref]
- K. Hönig (2017) Hypnose und Hypnotherapie in der Psychoonkologie. Nervenheilkunde 36: 981-987.
- G. H. Montgomery., J. B. Schnur., K. Kravits (2013) Hypnosis for cancer care: Over 200 years young. CA. Cancer J. Clin 63: 31-44. [Crossref]
- C. Flückinger., G. Wuesten., R. E. Zinbarg., B. Wampold (2010) Resource activation. Using clients’ own strengths in psychotherapy and counseling. Cambridge.
- K. Grawe (2007) Neuropsychotherapy. Routledge.
- N. Gelse (2023) Enhancing coping skills through brief interventions during cancer therapy – a quasi-experimental clinical pilot study. Front. Psychol 14. [Crossref]
- R. S. Lazarus (1974) Psychological Stress and Coping in Adaptation and Illness. Int. J. Psychiatry Med 5: 321-333. [Crossref]
- N. Schneiderman., G. Ironson., S. D. Siegel (1967) Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol 1: 607-628. [Crossref]
- S. Moorey., S. Greer (2011) Oxford Guide to CBT for People with Cancer, 2nd ed. Oxford University Press. [Crossref]
- M. de Vries., F. Stiefel (2014) Psycho-oncological interventions and psychotherapy in the oncology setting. Recent Results Cancer Res 197: 121-135. [Crossref]
- M. Wolf., W. Bongartz, Die (2009) Bestimmung des emotionalen Ressourcenpotenzials (BER)” – Psychometrische Überprüfung eines Tests zur Erfassung individueller emotionaler Erfahrungsmöglichkeiten, PPmP – Psychother, Psychosom. Medizinische Psychol 59: 5-13.
- A. Trösken., K. Grawe (2004) Inkongruenzerleben aufgrund brachliegender und fehlender Ressourcen,Verhal. Psychosoz. Prax 36: 51–62, 2004.
- P. H. Wirtz., L. Thomas., G. Domes., F. J. Penedo., U. Ehlert., et al. (2013) Psychoendocrine validation of a short measure for assessment of perceived stress management skills in different non-clinical populations. Psychoneuroendocrinology 38: 572-586. [Crossref]
- S. Temple (2017) Brief Cognitive Behavior Therapy for Cancer Patients, 1st ed. Routledge.
- M. P. Jensen., T. Adachi., C. Tomé-Pires., J. Lee., Z. J. Osman., et al. (2015) Mechanisms of Hypnosis: Toward the Development of a Biopsychosocial Model. Int. J. Clin. Exp. Hypn 63: 34-75. [Crossref]
- G. R. Elkins., A. F. Barabasz., J. R. Council., D. Spiegel (2015) Advancing Research and Practice: The Revised APA Division 30 Definition of Hypnosis. Int. J. Clin. Exp. Hypn 63: 1-9. [Crossref]
- G. Elkins., W. Fisher., A. Johnson., J. Sliwinski (2012) Clinical hypnosis for the palliative care of cancer patients. Oncology (Williston Park). 26: 26-30. [Crossref]
- J. B. Schnur., I. Kafer., C. Marcus., G. H. Montgomery (2008) Hypnosis to manage distress related to medical procedures: A meta-analysis. Contemp. Hypn 25: 114-128. [Crossref]
- G. Marchioro (2000) Hypnosis in the Treatment of Anticipatory Nausea and Vomiting in Patients Receiving Cancer Chemotherapy. Oncology 59: 100-104. [Crossref]
- G. H. Montgomery (2007) A Randomized Clinical Trial of a Brief Hypnosis Intervention to Control Side Effects in Breast Surgery Patients. JNCI J. Natl. Cancer Inst 99: 1304-1312. [Crossref]
- G. Elkins (2008) Randomized trial of a hypnosis intervention for treatment of hot flashes among breast cancer survivors. J. Clin. Oncol 26: 5022-5026. [Crossref]
- G. Elkins., A. Johnson., W. Fisher (2012) Cognitive Hypnotherapy for Pain Management. Am. J. Clin. Hypn 54: 294-310. [Crossref]
- K. Kravits (2013) Hypnosis: Adjunct Therapy for Cancer Pain Management. J. Adv. Pract. Oncol 4. [Crossref]
- D. Spiegel (1985) The Use of Hypnosis In Controlling Cancer Pain. Cancer J. Clin 35: 221-231. [Crossref]
- S. Daniels., DNP., ARNP., FNP-BC (2015) Cognitive Behavior Therapy for Patients With Cancer. J. Adv. Pract. Oncol 6: 54-56. [Crossref]
- M. A. Getu., C. Chen., W. Panpan., J. F. Mboineki., K. Dhakal., et al. (2021) The effect of cognitive behavioral therapy on the quality of life of breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Qual. Life Res 30: 367-384. [Crossref]
- K. Tatrow., G. H. Montgomery (2006) Cognitive Behavioral Therapy Techniques for Distress and Pain in Breast Cancer Patients: A Meta-Analysis. J. Behav. Med 29: 17-27. [Crossref]
- M. Ye (2018) A meta-analysis of the efficacy of cognitive behavior therapy on quality of life and psychological health of breast cancer survivors and patients. Psychooncology 27: 1695-1703. [Crossref]
- R. C. Ashton (1995) The Effects of Self-Hypnosis on Quality of Life Following Coronary Artery Bypass Surgery: Preliminary Results of a Prospective, Randomized Trial. J. Altern. Complement. Med 1: 285-290. [Crossref]
- A. Capafons (1998) Rapid Self-Hypnosis. Psicothema 10: 571-581.
- L. S. Milling., E. S. Randazzo (2016) Enhancing sports performance with hypnosis: An ode for Tiger Woods. Psychol. Conscious. Theory, Res. Pract 3: 45-60.
- R. S. Vealey (2007) Mental Skills Training in Sport in Handbook of Sport Psychology. Wiley 285-309.
- A. D. Eason., B. A. Parris (2019) Clinical applications of self-hypnosis: A systematic review and meta-analysis of randomized controlled trials. Psychol. Conscious. Theory, Res. Pract 6: 262-278.
- M. J. Diamond (1977) Hypnotizability is modifiable: An alternative approach. Int. J. Clin. Exp. Hypn 25: 147-166. [Crossref]
- F. H. Frankel (1976) Hypnosis: Trance as a Coping Mechanism. Plenum Medical Book Company.
- R. A. Bryant., M. L. Moulds., R. M. Guthrie., R. D. V. Nixon (2005) The Additive Benefit of Hypnosis and Cognitive-Behavioral Therapy in Treating Acute Stress Disorder. J. Consult. Clin. Psychol 73: 334-340. [Crossref]
- I. Kirsch., G. Montgomery., G. Sapirstein (1995) Hypnosis as an Adjunct to Cognitive-Behavioral Psychotherapy: A Meta-Analysis. J. Consult. Clin. Psychol 63: 214-220. [Crossref]
- M. E. Mendoza (2017) Randomized controlled trial of the Valencia model of waking hypnosis plus CBT for pain, fatigue, and sleep management in patients with cancer and cancer survivors. Psychooncology 26: 1832-1838. [Crossref]
- J. B. Schnur., D. David., M. Kangas., S. Green., D. H. Bovbjerg., et al. (2009) A Randomized trial of a cognitive-behavioral therapy and hypnosis intervention on positive and negative affect during breast cancer radiotherapy. J. Clin. Psychol 65: 443-455. [Crossref]
- C. Grégoire., M.-E. Faymonville., A. Vanhaudenhuyse., G. Jerusalem, S. Willems., et al. (2021) Randomized controlled trial of a group intervention combining self-hypnosis and self-care: secondary results on self-esteem, emotional distress and regulation, and mindfulness in post-treatment cancer patients. Qual. Life Res 30: 425-436. [Crossref]
- A. D. Eason (2013) The Science Of Self-Hypnosis: The Evidence Based Way To Hypnotise Yourself. Poole: Awake Media Productions.
- C. Grégoire (2020) Effects of an intervention combining self-care and self-hypnosis on fatigue and associated symptoms in post-treatment cancer patients: A randomized-controlled trial. Psychooncology 29: 1165-1173. [Crossref]