The classic and most common method of treating malignant tumors of the eyelids is surgical, which involves local excision of the tumor with a simultaneous reconstructive-restorative stage.
Almost all authors use a graft from the auricle as a graft for the reconstruction of defects in the skin and cartilaginous plate of the eyelid. The autograft is easily modeled in thickness and curvature. To restore the conjunctival cavity, we propose to use a lyophilized amniotic membrane.
The results of surgical treatment of 10 patients with ulcerative form of basal cell carcinoma of the lower eyelid, the stage of the disease according to TNM classification (2009) - T2a-3aN0M0 for the period 2015-2019 are presented.
By 12-14 days of the postoperative period, the engraftment of the skin flap was observed. Epithelial cells from the conjunctival fornix moved to the cartilaginous surface of the graft covered with a lyophilized amniotic membrane, which was confirmed by the results of a cytological study.
The use of a lyophilized amniotic membrane ensures the formation of the conjunctival cavity and obtains a good anatomical effect during reconstructive operations on the lower eyelid.
Basal Cell Carcinoma; Surgical Treatment; Eyelid Reconstruction; Lyophilized Amniotic Membrane Flap
Basal cell carcinoma prevails in the malignant tumors of the eyelid skin (94.7%), less common are squamous cell and metatypic carcinoma (4%), adenocarcinoma of the meibomian gland (0.7%) and skin melanoma (0.6%). Primary multiple lesion occurs in 6% of patients. The treatment frequency in advanced stages of the disease reaches 12-15%, despite the diagnostic availability of the eyelid skin tumors and adoculus conjunctiva. This is associated not only with late treatment, but also with late correct diagnosis.
Surgical treatment is necessary to recognize as classical and most widespread method, that involves local tumor excision with simultaneous reconstructive and recovery phase [1, 2].
At the current stage of the oncology development the surgical method has become much more aggressive. Expanded surgery is increasingly used to improve treatment outcomes. Radical operations are inevitably associated with the formation of significant cosmetic defects in periorbital tissues. Soft tissue deficiency and violation of their functionality leads to retraction and deformation of the eyelids with the lagophthalma formation. Progressive scarring in the postoperative period creates the conditions for fornix overgrowth, eyelid inversion and the development of pathological changes in the surface of the eye anterior segment.
Functional and cosmetic rehabilitation is a major ophthalmplasticity problem of patients with cicatricial deformations of the eyelids and periorbital zone [3.4].
After neoplasm removal small full-thickness defects (no more than one third of the eyelid) are replaced by moving the flaps from a healthy eyelid. If the defects are more than one third of the eyelid, it is problematic to recover not only the skin, but also the tarsal plates and the appropriate conjunctival cavity formation [5, 6].
Skin surface restoration usually occurs by free skin flap auto transplantation. The cartilage layer is more difficult to recover. Some authors use cadaveric cartilage. But the autologous auricle cartilage from the fossa or antihelix is used most often [7]. All authors agree on the use the auricle cartilage as reconstructing graft for insignificant defects in the eyelid cartilaginous lamina. The auto graft is easily modeled in thickness and curvature and is simple and convenient to recovery. It should be noted that the donor cartilaginous layer is important to isolate from contact with tear secretion [8].
The eyelid posterior surface restoration can occur through direct cover the defect with the autoconjunctival flap, as well as by transplantation the lip mucous membrane. The direct cover of the defects with autoconjunctival flap has some disadvantages: the possibility of using insignificant defects, deformation of the conjunctival fornix due to excessive overstretching and subsequent scarring. The disadvantages of the lip mucous transplantation are excessive flap reduction and severe scarring [9].
To cover the underlying tissues and for the conjunctival cavity formation, we propose to use an allogeneic biological material - a lyophilized amniotic membrane.
The lyophilized amniotic membrane does not have viable cells on its surface.
However, lyophilization preserves the basement membrane and avascular stroma intact. This allows the lyophilized amniotic membrane to be the substrate for the epithelial cells growth, as proved by the regeneration of the corneal and conjunctival epithelium in various diseases and damage of the anterior eye segment surface.
The purpose of this study is to explore the possibility of using a lyophilized amniotic membrane as part of the graft in eyelid reconstruction after full-thickness eyelid resection.
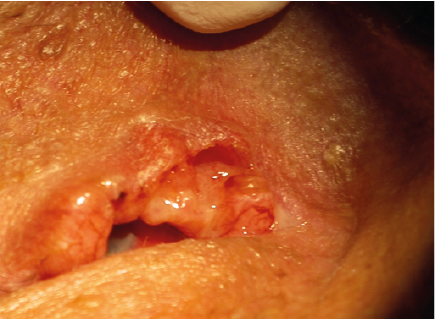
The surgical treatment results are studied in 10 patients with ulcerative basal cell carcinoma of the lower eyelid between 2015-2019, disease stage according to the classification of TNM (2009) - T2a-3aN0M0 [10] (Figure1). It must be noted, that neoplasm growth after cryodestruction occurred in one patient from this group.
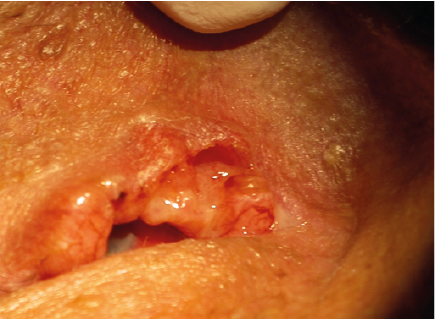
Figure 1: Ulcerative Basal Cell Carcinoma of the Lower Eyelid
Full-thickness resection more than 1/2 of the eyelid was performed on all observed patients. The minimum size of the excised tissue horizontally was 18.0 mm, the maximum up to 25.0 mm. The neoplasm was excised for the whole thickness of the eyelid with «Surgitron» radio wave knife. The resulting biological material was sent for histological examination.
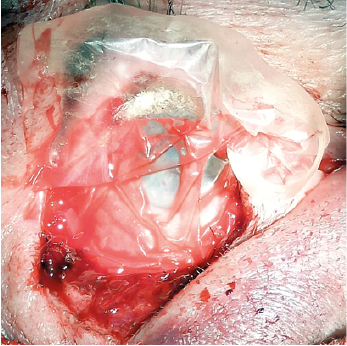
In order to repair the tissue defect, plastic surgery was performed with a skin-cartilaginous flap on the back of the auricle. The cartilaginous graft was fixed with interrupted sutures to the preserved parts of the tarsus, or to the palpebral ligament fibers. The dissected fragments of the orbicularis oculi were fixed on the donor cartilage surface after partial skin flap separation. The conjunctival cavity was reconstructed by the lyophilized amniotic membrane. The amniotic membrane implant was inserted under healthy conjunctival tissue and stitched with a continuous suture 8/0 (Figure 2). In all cases, the operation ended with suture graft fixation to the edge of the upper eyelid.
All patients were observed in the postoperative and longer-term period up to two years.
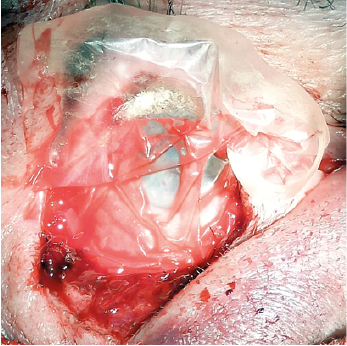
Figure 2: The Amniotic Membrane Implant Was Inserted Under Healthy Conjunctival Tissue and Stitched With A Suture 8/0
In all cases, the skin flap acquired a pale pink color in the operated patients, by the 12-14th day of the postoperative period. Deformation or lysis of the cartilaginous layer was not observed.
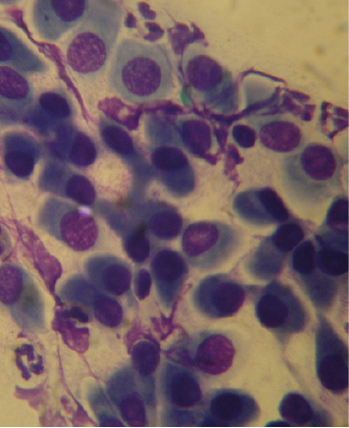
The transplant cover with a lyophilized amniotic membrane and its gradual lysis facilitated the movement of epithelial cells from the conjunctival fornix that is confirmed by the results of a cytological study. Epithelial cells typical for the eyelid conjunctiva from the posterior graft surface were determined on cytograms 2 months after surgery (Figure 3).
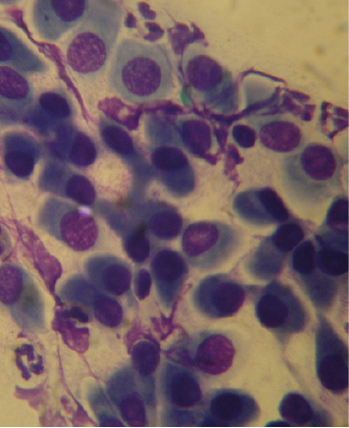
Figure 3: Cytogram 2 Months after Surgery from the Posterior Surface of the Graft. In the Preparation, Layers of Monomorphic Conjunctival Epithelium, Single Elements of Inflammation, Mucus. Magnification X 100. Azur Eosin Coloring
It was observed complete palpebral fissure closure after the posterior layer reconstruction with a free skin-cartilage flap and lyophilized amniotic membrane. However, the lower eyelid was atonic, slightly mobile. The posterior layer was covered with pale pink epithelium. The inferior conjunctival fornix was uneven in depth, without coarse cicatricial deformation.
In the long-term postoperative period, 30% of cases (three patients) had the tumor relapse, what can be explained according to the results of histological research by the excision of the neoplasm not within healthy tissue. Corrective surgery because of a partial lower eyelid inversion was completed in a patient.
It should be noted, that all operated patients had the full conjunctival surface forming. Conjunctival regeneration occurs on the cell-free biological substrate of the implant, made of lyophilized amniotic membrane, which is gradually lyzed enriching the conjunctival sac with glycoproteins, interleukins, and growth factors [11]. These substances enhance the proliferation, migration, and differentiation of regional epithelial stem cells, prevent apoptosis, and inhibit the fibrosis development [12]. Biomaterial replacement of the lyophilized amniotic membrane ends by the 10th - 13th day of the postoperative period with the conjunctival forming that is tightly adjacent to the eyelid cartilage layer and forms a single whole with the healthy conjunctiva.
The results of the application of the lyophilized amniotic membrane for the surgical treatment of the eyelids confirm its ability to enhance the movement of epithelial cells and their fixation in the defect zone.
The use of a lyophilized amniotic membrane suppresses excessive scarring of the conjunctiva and ensures the formation of the epithelial layer on the cell- free matrix that allows getting good anatomical effect during reconstructive operations on the lower eyelid.
- Brovkina AF (2002) Ophthalmic oncology: a guide for doctors. M Medicine 442.
- Pear YO, Ismailova DS, Rizopulu EF (2013) Plastic defects after resection of the eyelids with benign and malignant neoplasms. Bulletin of Ophthalmology 129: 44-49.
- Vasiliev SA (2002) Plastic surgery in oncology. Chelyabinsk: ChGMA 209.
- Verbo EV, Nerobeev AI (2008) Face reconstruction with revascularized autografts. M Medicine 108-109s.
- Filatova IA, IA Filatova, SA Shemetov (2016) On the correction of post-traumatic eyelid kolobom IX Russian National Ophthalmological Forum. Sat scientific 1: 85-87.
- Nemec I (2016) Upper eyelid injury with partial loss. Case report. Acta Chir Plast 58: 82-84. [Crossref]
- K Hashikawa, S Tahara, M Nakahara (2005) Total lower lid support with auricular cartilage graft. Plast Reconstr Surg 115: 880-884. [Crossref]
- Grishchenko SV, Vissarionov VA, Filatova IA, et al. (2012) Modern possibilities of free tissue autotransplantation in reconstructive surgery of the eyelids and periorbital region. Ross honey Journal 3: 23.
- L de Sousa, I Leibovitch, R Malhotra (2007) Techniques and outcomes of total upper and lower eyelid reconstruction. Arch J Ophthalmol 125: 1601-1609. [Crossref]
- Sobin LH, Gospodarowicz MK, Wittekind C (2009) The TNM classification of malignant tumours 8th edition. Wiley-Blackwell.
- Champliaud MF, Lunstrum GP, Rousselle P, et al. (1996) Human amnion contains a novel laminin variant, laminin 7, which like laminin 6, covalently associates with laminin 5 to promote stable epithelial-stromal attachment. J Cell Biol 132:1189-1198. [Crossref]
- Keelan JA, Sato T, Mitchell MD (1997) Regulation of interleukin (IL)-6 and IL-8 production in an amnion-derived cell line by cytokines, growth factors, glucocorticoids, and phorbol esters. Am J Reprod Immunol 38: 272-278. [Crossref]