Purpose: Quality of live is for everyone different but everyone wants to be independent. People with dementia are no different and want to walk and sit where she want. But often this isn’t possible for them, are much workers in this field think. The purpose of this article is to assess a person with dementia and see or after that assessment and treatment can be developing that can change something.
Method: We use an assessment–form that is use by the assessment of people with dementia and is an important part of education of therapist as specialist on this field of psycho-geriatric. This is an assessment that as three parts.
Part 1: What can him!
Part 2: How do him it!
Part 3: Why he act so!
Result: Assessment of our Case ( Mister C.) give an picture that he act on level that was lower because of the combination of pathological tone and synergy and the loss of muscle power and coordination.
The treatment that he receive, wasn’t pointed on that restriction but was an treatment that consist out walking with his rollator frame and was sometimes an aerobe stimulus.
Conclusion: To treat this people on the right level an assessment is necessary and a good treatment plane because that we can help the quality of life for a longer tine hold on higher level. Authorship credit: “Criteria authorship scientific article” has been used “Equal Contribution” (EC)
Dementia; Assessment Physical Therapy; Senior Fitness Test; Treatment
Strange fact is that when people with the diagnosis dementia are seldom total physical assessed. Often is there a program rom assist by the problems that occur when the disease progressed. Still investigation has revealed that walking and balance problems occur almost 10 years for the diagnosis dementia is done [1]. Furthermore is it known that people with Mild Cognitive Impairment (M.C.I.) move less [2, 3], but that is it very important to known why and what the consequences are for the body/mind possibilities.
When there is an problem with movement in the ADL context than is an consult and treatment through an physical therapist important and that is also the moment to do an good and total assessment to invest what the problems are at that moment and where the difficulties lies or maybe will lie in the future.
Of course this has to be done by all persons that start with a physical treatment but by this group it is more important because the disease makes a total screening almost impossible and then it is so important that there is a moment in which that has done and that others can see back.
Also the connection with the ADL and even the movement that are crucial to move and live independent in their own home is essential. Too often will that home be a place where all kinds of aids where installed without an assessment or that with give a contribution to those independent living possibilities.
A nice example is the rollator frame. Much of the elderly has such an device without that there is an person that has look what the best type are [4] and what the reason was that this person feels less secure without such an support device. That why is so important because that need for an assessment but too often the answer is an aid that makes the problem not lesser but less visible and there are assumptions [5-7], that the balance is faster decrease as before. That as a result of the support that makes the job easier for the legs and that decrease the strength and the coordination and also the body perception.
That last aspect is so important because we know That the body perception is change in an lying [8] position by this disease but also that there are alteration in stand and balance position [9, 10] and then standing devices [11, 12] have also an negative impact and therefore it is so important to know how that system is at that starting moment. Even the sense under the feet in all its different aspects[13] is at that starting point essential because that will explain why someone don’t lift his feet so often.
An special aspect is the tone that is an symptom of this disease that alter much and knowing that this is present and on which scale is even important as the power or the coordination. Because a tone increase, decrease the selectivity and therefore has a great negative impact on that power and coordination and we must find a solution to control that tone increase as long as possible and how we doing that.
Cognitive aspect is also important, not only knowing what the possibilities are of the brain but also to know what for a person this patient was before the disease “stroke” him. That social- cultural aspect is important because despite the changing in character that can occur, often are the person before still there and an quit person that isn’t use to get attention, will that often do the same as before and that can give isolating in an group.
That cognitive aspect is also essential to learn to deal with this people. Often there is still a great amount of verbal coaching what for this people isn’t possible anymore. To get the message over there must often be other ways use. As “being a copycat “or seduce the patient to move with you. Negative experiences have often more impact than we think. This experience will stay longer in this damage brain [14-16]. Therefore make it always a positive experience. Laughter is so important that this must be a part of the treatment and the assessment is the moment to search for a part history and make the world for them “visible“ [17-19].
Be prepare when the treatment get started on all fronts and then is the cognitive aspect essential because the capacity[20], is on physical and mental restricted and we must know before we start what that capacity border is and this will change when the disease progressed.
To introduced and explain the assessment form we use a casus of a gentlemen that has a diagnosis dementia and P.S.P (Progressive Supranucleaire Paralyse). The disease is progress in the last year that a hospitalization in a nursing-home was necessary. Especially his walking and balance capacity was decreasing but it was good possible to do the assessment test. Still it isn’t done in one session, mostly is that not possible, but in 4 sessions of 20 minutes.

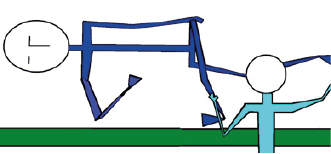
Photo 1. Mister C. is on this photo about 76 years old and he is working his whole life on a farm. Not a farm of his own but that of his brother. He has received about 5 years ago the diagnosis P.S.P. and in the same year there was a diagnosis dementia. His ability to walk independently and especially is balance was decreasing rapidly and he was dependent of a rollator frame to walk in the rooms of the nursing home. As so often is walking in a Nursing home with a rollator frame no sign that there is a problem with his balance. In the years before, he has received treatment at home but the data about that treatment were so poor. Still in the conversation he was able to perform, he give as his greatest problem not the balance or the walking capacity with the rollator frame, but his greatest problem was that he wasn't ’able to get to the toilet on time. That was a problem, according his story that he cannot stay at home and the greatest problem was coming out his bed. That asked so much effort and time that he was often too late.
It is often important the wishes of the patient to know because often will that deliver a much higher motivation as that problem is the focus of the treatment. But only the focus on that problem makes a good assessment often to small and isn’t often deep enough to get behind the reason of this less functioning. Another strategy that is follow is the same why so often a walking aid is given. Given a walking aid isn’t wrong but without a search why that aid is necessary is essential.
Often we see that by problems in and out bed that there are aids installed to make moving in and moving in and out make easier. Often that result is obtain for an short time and the most comment solution in nursing home is that the person gives an ring and the nurse is coming to assist. [22-25].
Observation form (Rakt-concept) (Casus Mister C) [26].
1 Data patient:
Name: Mister C, Day of birth; 14-04-1937
Diagnose: PSP / Dementia
What can the Person?
The first item that we will assess is what this person can. Now we have a good image what the person can on his own and where he needs assistance. Now …by what only yes or no, a little remark is sustained. Table 1 start with movement in and out bed and we can choose out 4 possibilities. Independent: that is no assistance necessary and is the situation safe.
Supervision; he is able to do it on his own but this is according the person that do this observation form not safe.
Assistance / Facilitation: There is a difference between this two. Assistance means that some of the body weight is take over by another person, but facilitation means that we create a situation in which the movement is better possible but still he is dependent of another person.
Not possible: The person cannot perform this movement.
Clinimetric: There are by this chapter = WHAT = a lot of possibilities to do measurements and make a basic measurement box what this person on that moment can do. Often good comparison material at the start of the treatment [27-31].
The X-sign is the sign what mister C performed.
Table 1
Table 2
Table 3
Table 4
Table 5
WHAT == Activity – level
Summary; it is clear that his possibilities in and out bed are less and asked almost all for an assistance or supervision. And supervision gives often then image that the person that does this assessment isn’t sure that he can do this safe. Standing and sitting him manage that but again with supervision and we must yourself the question: Is that possible out all chairs, bed and toilet”.
Than we come by the walking part, here is an obvious decline in capacity. He walks with an aid (rollator frame) we know that he got that several months ago when he lived in his home and this aid especially use when he walks outdoor. But when he was hospitalized, he came not out door till now.
Still the speed and the distance is very low and we perform an TUC (Time Up and Go -test) and that was almost 16 sec. Especially the standing up part on the standard chair asked for much time and he performance by the turning point was also slow.
Here we see again the combination of difficulties of movements in and out bed and problems with the TUG test [20]. Therefore was the relation that the muscles that play an mayor part by the movements in /out bed are also important by standing up, turning and walking with speed. Or and there is more tone increase as reported by the therapist that treat him at home.
Further sometime less functioning in his right shoulder and also his cervical spine and the mouth and tongue movement are less as we expected.
Trunk Control Test: 87 point of the 100.
Barthel Index: 10 point of the 20.
Berg Balance Scale: 31 of the 56 and below 45give and risk of fall danger.
10 meter Walk Test: 19-20 sec
Functional Ambulation Categories: 3
Motricity Index (leg):-
Stop Walking When Talking: positive, he stand still when someone spook with him.
Motricity Index (arm): Left 99 (max. Right 85).
One leg standing; 3 sec with eyes open
Rikli & Jones: 7 items
- 30 sec. Chair and stand ( normal for is age 11-17) = max 8 (far below)
- Arm curl ( normal for his age 13-19) = 15 (good)
- 2 min steps test ( normal for his age 73-109) = 30 ( far below)
- 6 minutes’ walk ( normal for his age 470-640)= 250 ( far below)
- Chair sit and reach ( normal for his age -5,5 ) = 10 ( rigid)
- Back Scratch ( normal for his age -9.0) = 15 (rigid)
- 8 foot Up and Go (TUG) (normal for his age 7.2 – 4.5) = 16 ( far below)
We have an lot of measurements in which the picture is created that he has difficulties and often assistance needed to get out bed, out the chair and that walking is independent but with an rollator and often with supervision. There are also clear sign that the balance is poor and that there is less mobility or rigid or paratonia. But we don’t know why and what structures have an great part in the problems. That we must assess in the WHY part. But first we look HOW he moves because the way he try to solve the problems can us give an sign where we must assess extra. Furthermore we will look what he gives as a great problem.
Where will you focus on in this assessment? (What is the assistance call of the patient)
His greatest problem was that he wasn't ’able to get to the toilet on time. That wish, contain a lot of different elements that are all opposite and range from movement in bed over walking till sitting down on a toilet. There are not only a lot of different movements but also a lot of different environments that claim adaptation for then movement strategy of this patient.
- Movement in bed. That we know isn’t all independent there is an starting problem that cause time
- Movement till sit on the edge of the bed. Again we know that this problematic but we know not WHY.
- Standing up from the bed edge. Standing up from an chair was possible but is that also the case from an bed and are there bracing elements of the bed in an nursing home [39].
- Standing up and grasping the walking aid. And walking to the toilet.
- Standing for the toilet and undressed.
- And sitting down on the toilet.
Of course is the standing up, the care for him to be proper and to dress him necessary to get the picture complete. But in this assessment we focus on the way till he sits on the toilet.
What now very important is HOW he performed that we compare with normal movement done by elderly that have no neurological symptom because that is the best way to find the differences [4, 40].
Common elements of this task.
How functioned the patient?: Act the patient safe, impulsive, scared, over active, has he think on his limits ?
- Mister C.is perfect capable to control the situation and never he take risk that he cannot control. But that makes all movement slow and that asked for enough power and selectivity.
How is he orientated on his task? Is the preparation, goal attention, spatial orientation (the position of his body in the room, distance, direction, in handling of objects and the pace and function of this object and has he eye for surrounding.
- Again, this is good and he search for alternatives to reach his goal.
How is the execution of the task? Temporal organization, initiation of the movement, the sequence, procession and the completion of this task.
How move the patient? Is his movement fluently, coordinated, with variation and with enough power?
- His movement are slow, to slow and it is important to find the reason for this because that cost a lot of power.
Is the patient capable to adapt on changes? When the surrounding change how he reacts? On the orientation, the execution and completion of the task. What is happen when there is an increase on the task trough stress or double tasking?
- This is present but minimal. He tried it on another way but that will never create a better performance. But the environment presses him often to choose for one strategy because other and strategy asked for an adaptation of the environment. As example standing up must always performed with the hand on the side of his body to push himself up. Support on the front and use the arm to pull himself to a standing situation isn’t possible on his chamber and also not on the toilet [39-42].
Describe two tasks that is representative for his activity level. (1. Coming to sit on the edge of the bed and 2. standing up).
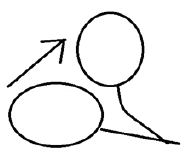
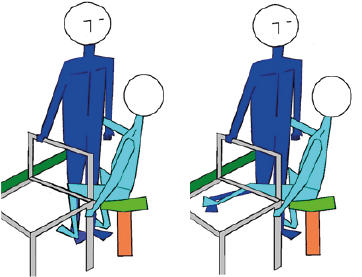
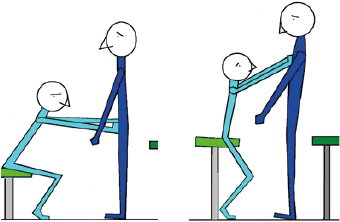
First: Coming to sit on the edge of the bed and we have search for a comparison between this case and an elderly that hasn’t neurological problems.

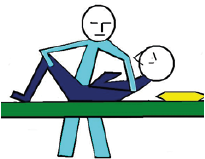
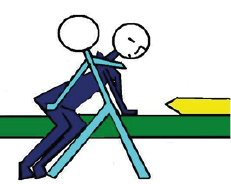
Photo 2. In the what of this assessment we say that he wasn’t capable to do this without pulling on the blankets. That makes these effort 12 points on the T.C.T. scale. This position he stays in balance with the whole weight of his body on the right elbow. Than he use the other left arm to push on the bed behind his back or he use this hand/arm to pull on the blankets and get so the weight of his elbow and can stretch his right arm to push him to an sitting position (on photo 1 we see him when this is succeed.
Head (Pay attention on the attitude of the head but also on the place and structure of the tongue bone/tongue and the neck muscle on the front).
The head position is in the middle. There is no shortening of the cervical trunk in the direction that the movement must go. The front of the neck is visible therefore we cannot see what the muscle here does and how the tension is that maybe have an influence on the swallowing possibilities.
Trunk: (where start the movement in the trunk (upper or lower trunk).

Photo 3. Coming to sit on the edge of the bed. And we see immediately the differences with photo 2. The amount of effort that Mister C needed to get on the edge of the bed is much larger than the man on this photo. This person has the time and the opportunity to stay an few second in this position for this photo and Mister C. must stay in that position to get his arm free to push or pull to get in an erect position. One of the symptoms of neurological diseases and certainly dementia is a slow movement performance that isn’t changeable easily.
What we see in the cervical trunk we see also in the thoracic- and lumbar spine. No shortening of the spine on left side and that is an indication that the spine cannot shorten because the support on the elbow makes it impossible
Shoulder / arm / hand:
It is clear that the movement – coming to sit on the edge of the bed – is done through the great work of both arms.
Pelvis / leg / Foot:
In the hip we see that the side with weight has exorotation and the other side stand more in endorotation and when we pay attention on the feet than are they in an plantar flexion.

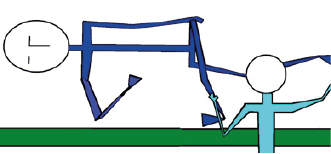
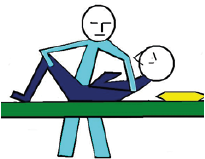
Photo 4. Mister C performing standing task from his wheelchair on his own way. There is place an chair in front of him but nobody has instructed him to use this chair because we want to know what his most use strategy was and how he performed that. Below the HOW is further explained. But what we see in this photo is that this cost power and attention to make it possible and that he must do a few attempts to get in standing position. Again we see that he isn’t capable to accelerate his movement and that the strategy he use is always the same and that is often a sign that his environment is poor [20-22]. The possibilities of the environment to functioning optimal aren’t often not a part of assessment but people with dementia are dependent of those possibilities to hold their dependency.
Second: Standing up

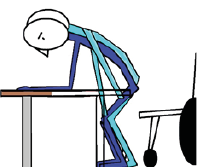
Photo 5. We place a bench in front of him and place him on an normal chair. Normal qua height but also qua form, meaning that the back part of the sitting part is almost equal with the front. The table was 10 cm lower than the table in his apartment. We asked him to grasp the edge of the bench so far that the elbow was supported on the bench. And look he has placed his feet behind the knee in the perfect position for a standing up movement. That we haven’t asked him only grasp the edge.
Head:
The position of the head is fixated to an area in front of the feet. The rest of the room or what there is behind the chair isn’t “important” and get no attention. The whole capacity of the eyes is focus on that small area.
Trunk:
The movement of then trunk to the front is too short and the amount of “vorlage” is too small and the movement of the feet to the back is to early stop. Normally will elderly move without load on the hand to the front and that will give a good foot placement. Now is the trunk movement stop too early because of the weight bearing of the hand and thus also the feet and is a good placement of the feet not possible. To illustrate that he has still the capacity to make a good “vorlage” and therefore a good foot placement look to photo 5.
Shoulder / arm / hand:
The use of the arm is great and that will have consequences for the gleno-humeral joints, but this will also restricted the movement of the trunk to the front and makes the standing up strategy heavier and dangerous.
Pelvis / leg / Foot:
A very important phenomenon is that both fore foot are active in dorsal flexion. A sign that his balance system has notice that his weight is too far on the back side of the feet and that he is out of balance. That will give a problem when he standing with support on his hands because when he cannot change the position of his feet, he will fall back in the wheelchair. Go and grasped the chair or a rollator frame makes than a “dangerous “act.
This performance cost and lot of strength not only physical but also mentally and therefore stand by the WHAT part that the standing up occurs under supervision. Many people that car for him, will asked him to call for help when he want to stand up and that makes him less dependent and will restricted him in his wish to go the toilet on his own.
Therefore this strategy isn’t appropriated for him with his possibilities and let’s looks as we the environment change.
We have seen that the way he is coming to sit on the edge of the bed and the standing up movement, that he must use all kind of alternatives to get the job done. Much must be done by his arms and hands and that pointed out that his lower trunk /legs have difficulties with that job. Furthermore is the speed of Mister C. always very low. It looks that he isn’t capable to speeding up. He understands the instructions and commandos and search for a solution and uses every think he has but he has no answer on his limitation.
He wish get out the bed and walk on his own to the toilet asked very much of him and we have look to two part of this whole wish and then we see the problems but we don’t know WHY and therefore is a treatment not possible. It has no value this to train on his apartment without knowing where the greatest problems lie and makes also a task-specific treatment with this information not possible. The whole Battery of test we have done gives us an image but tell us nothing about the WHY.
WHY move the patient on this way ? Analyse of the performance.

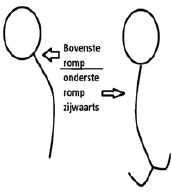
Figure 1. This figure must be use during the whole assessment but especially in the WHY part. WE want to know what hurts, is difficult or “dangerous” according the person
Furthermore is it important that we know how much energy this person has needed to do the assessment because that gives us an indication how heavy it is for him. Of course use this also in the WHAT and HOW part. [42, 43].
Placing (selectivity investigation): Placing is an passive movement from one point to another and we feel how easy that goes or that there resistance. Than as we have reach that point, we asked to hold that position. And then we observe how good that is done and the same position without little movements to set the position (tuning) and even a little resistance is be given in that position to feel how good that position is hold. Placing- Hold- (Tuning) Hold with resistance. This gives an indication about the tone and the selectivity. This is often one in supine position certainly for the legs but can in every position. Doing it in supine position asked for an extra attention because difficult in supine position will be correlated with very difficult in sit of standing position because of the gravity. The trunk placing is very difficult but the best result is reached in sit.
Head: The results are that of the assessment of our case Mister C.
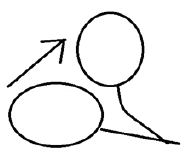
Figure 2. Placing –holding and holding against resistance
Placing from supine to optimal cervical flexion (figure 2) isn’t smoothly. There is resistance and deviation to right. Holding the head in optimal flexion isn’t possible. The head goes back in an antero-position. Resistance is therefore not possible.
The movement gives resistance and that is most on the end of the head. When we asked to hold the head in that position, his head goes an little back in extension in the highest cervical spine. The movement rotation and lateroflexion let see that to the right this is more problematic.
Trunk –in sitting position
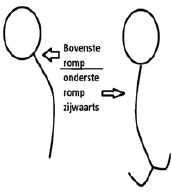
Figure 3. In sitting is gravity present but in supine position that asked to much from the stomach muscle and that is often not possible. First upper trunk flexion (eccentric) and back and lateroflexion also first eccentric. Thus this isn’t passive but relaxation. Lower trunk extension to the front (concentric) and flexion (eccentric) and then lateroflexion asked for a movement sitting on one buttock with an elongation and that asked a lot of power and coordination. Rotation in upper and lower can also access and we do it by placing our hands on the shoulder and “place” the body to an hold position and give resistance at the end and feel what that resistance is. Through the sitting position is passive “placing “not possible.
Mister C. scored by this test for the upper trunk flexion: difficult and slow . End position he can hold but with no resistance. Shortening to the left (relaxation of the right side ) with variable resistance and the end position has no resistance power. Shortening to the right ( left eccentric relaxation ) was better and no there was what resistance possible by the hold. Still the movement to the front and back and left and right shortening and back had more resistance as normal.
Lower trunk to the front gave immediately a resistance (fear!) because he sits on the edge of a bench with the feet free. There where he stops (Hold) was resistance not possible, he move back. Go to an flexion was also minimal possible. Placing him to the left or right buttock was impossible. Every time he starts in the upper trunk.

Figure 4 and 5. An example of placing – holding (resistance) of the arm. We choose for two positions for the gleno –humeral joint, one concentric and the other eccentric. Furthermore we trie to differentiated between the two pathological synergy beside the resistance against the passive movement and the holding possibilities.
Mister C. Score:
Figure 4 right arm placing was almost normal but holding was difficult in all three joint and resistance not possible. Figure 5 asked in the gleno-humeral joint for a different route because it hurts. Position hold was difficult and again never he could hold the joint position directly correct.
Left was almost the same but now there was no different route necessary but the placing was almost normal and the holding again difficult and resistance thus not possible.
It looks that there are influence of synergy are present to hold the joint in the end position as in the figures 4 and 5.
Leg in supine position
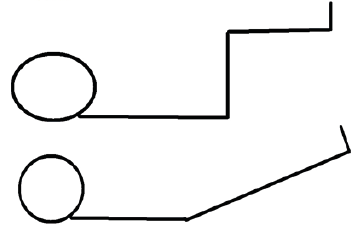
Figure 6 and 7 Again we search for position that is difficult as there is pathological synergy be active. Figure 6 asked for a hip placing and holding in an hip position of 90 flexion with the mid-stance for the abduction-adduction and also the rotations. Figure 7 is a heavy position because this asked for core stability but also an dorsal flexion in an almost complete extension pattern [44-46].
Mister C. Score
Rigth leg: Figure 6 placing was relative heavy, both elements were there; heaviness (low tone) and resistance (high tone). Holding wasn’t possible in all three joints. In the hip there was exorotation with abduction and the flexion was too much. Knee flexion could he not hold the 90 degree and also the dorsal flexion. Holding with resistance was therefore not possible.
Figure 7 placing were again difficult there was resistance that increase as we get to the hold position and holding wasn’t possible in all three joint but the dorsal flexion was the first component that decreases.
Left Leg; Figure 6, the image was somewhat better than right but the holding was again bad. Also in figure 7.
The resistance on placing was high in head, trunk and legs. In the arms was this almost normal except the right shoulder but there is a mobility restriction. But holding was bad in head, trunk but especially in the legs that pointed that the pathological synergy is positive. And test in an open chain makes control over the joint more difficult.
The selectivity is less through a neurological disease and the tone/synergy in the lower trunk and legs are clear changing.
Why move the patient on this way? Analyse of the performance.
Amount of resistance. Passive assessment of the tone investigation done in supine position or it will be described.
MAS- P: Modified Asworth Scale – Paratonia (Waardenburg and co). [47,48,49,50]
0 = neither resistance nor assistance to passive movement.
1 = Slight resistance during passive movement.
2 = More marked resistance to passive movement.
3 = Considerable resistance to passive movement.
4 = Severe resistance to passive movement, passive movement is impossible.
The tempo of movement is that of MAS assessment. A speed of 4 numbers at knee or elbow to go from full flexion to full extension. That speed is the base. By no resistance (level 0 or level 1) we can search further trough an increase of speed according the Tardieu scale. Stand in the score a T, than we accelerate we the speed and feel we resistance. The movement is being done passive and that means that we test the antagonist of the movement.
Score of Mister C. tone investigation by passive movement.
|
Movement |
Resistance |
|
Movement |
Resistance |
Head |
Flexion |
2 |
Elbow |
Flexion |
Left Right
2 2 |
|
Extension |
1 |
|
Extension |
1 1 |
|
Laterofl. left |
2 |
|
Supination |
2 2 |
|
Laterofl. right |
1 |
|
Pronation |
1 1 |
|
Rotation left |
2 |
Wrist |
Ulnair deviation |
1 1 |
|
Rotation right |
1 |
|
Radial deviation |
1 1 |
Trunk Sit |
|
|
|
Dorsaal flexion |
1 1 |
Upper |
Flexion |
2 |
|
Palmair flexion |
1 1 |
|
Extension |
1 |
Fingers |
Flexion |
1 1 |
Whole trunk |
Rotation left |
2 |
|
Extension |
0 T 0 T |
Whole trunk |
Rotation right |
1 |
Thumb |
Extension |
1 1 |
Lower |
Flexion |
2 |
|
Flexion |
0 T 0 T |
|
Extension |
1 |
|
Opposition |
0 0 |
Whole trunk |
Laterofl. left |
2 |
|
Abduction |
0 0 |
Whole trunk |
Laterofl. right |
2 |
|
Adduction |
0 0 |
Arm |
|
|
Hip |
Flexion |
2 2 |
Shoulder blade in side lying |
Elevation |
Left Right
2 2 |
|
Extension |
1 1 |
|
Depression |
2 2 |
|
Abduction |
2 2 |
|
Latero rot. |
1 1 |
|
Adduction |
1 1 |
|
Media rot. |
2 2 |
|
Endorotation |
0 T 0 T |
|
Adduction |
2 2 |
|
Exorotation |
0 T 0 T |
|
Abduction |
2 2 |
Knee |
Flexion |
2 2 |
Shoulder |
Anteflexion |
1 2 |
|
Extension |
1 1 |
|
Retroflexion |
1 2 |
Ankle |
Dorsal flexion |
2 2 |
|
Abduction |
1 2 |
|
Plantair flexion |
1 1 |
|
Adduction |
1 2 |
|
Inversion |
2 2 |
|
Exorotation |
1 2 |
|
Eversion |
1 1 |
|
Endorotation |
1 2 |
Toe |
Flexion |
1 1 |
|
|
|
|
Extension |
3 3 |
Summary tone assessment:
There is in the whole body a tone increase and there is a tone increase in the agonist and in the antagonist. That is a sign that this is paratonia [51] when in the agonist as in the antagonist is the tone increase. In the hand was the tone almost normal but when we increase the speed than the resistance was there only in the thumb stay that normal. Furthermore the tone is highest in both legs and that correlate with the signs of synergy we say by selectivity assessment. Extreme is the extension of the toes gives so much resistance.
Still it is important to differentiate the tone from other forms of resistance or mobility loss. That we do in the next part.
Which form of resistance there is by the passive movement?
1. Stiffness. = decrease of viscose –elastic in the tissues (not neural changes of the nerves)
Describe where you feel this stiffness = the stiffness that means an increasing of the resistance at the end of the movement excursion. By the MAS-P test the whole movement excursion must be made by 0 -1 and 2, but it is important to feel what this resistance do at the end of excursion because this can be a sign that there is other reason of resistance. Most clear was the right shoulder and the neck movements (rotation and later flexion to the left). The tone of the toes toward extension gives an increase of tone and the end isn’t reach.
2. Contractures of the muscles (Not – nerve):
Describe where you feel that muscle decreases = No signs where there. Except the toes but is this a contractures (irreversible) or loss of sarcomeres of cross junctions [52-55]. This cans also a sign that the balance holding is a great problem and that the clawing of the toes is necessary to create the optimal perception of movement under the feet.
3. Rigidity (= Lead pipe phenome)
Is there an rigidity to feel = no
4. Paratonia, Tone is high in agonist and antagonist.
Is there paratonia YES
Describe where you feel it: Almost all movements gave resistance and also the antagonist. This is sign that the paratonia is everywhere except in the thumb.
5. Hypotonic = flaccid = muscle tone to low No signs where there.
6. Changing tone (ataxia, chorea, athethosis) No signs where there.
7. Hypertonia = (Jackknife phenome)
Clonus =No signs where there.
Hyperreflexie: -----
Association reactions: ----
Tonic (static) reaction– activity [46].
Local reactions = Positive support reactions in the legs
Segmental reactions = Cross extension –flexion reaction
Total reaction = By standing up performance sometimes an Symm. Tonic. Neck Rection
0 = feeling is good
1 = Minor disturbances
2 = Moderate disturbances
3 = Severe disturbances
Sensoric / perception, what feels brain of Mister C.?
Test of the sense and perception.
|
Surface
Sense |
Tuning Fork
125/64hrz. |
|
|
Sense in muscle and joint.
(Depth sense / Proprioception) |
|
Pain
Temp.
Pressure |
Gnostic
Sens. |
Extinction |
Fine sense and
2-points-discr. |
Body position
and
Control movement |
Mirroring |
Head |
0 |
0 |
0 |
0 |
1 |
- |
Trunk |
1 |
1 |
0 |
1 |
1 |
- |
Arm |
1 |
1 |
0 |
1 |
1-2 |
1 |
Hand |
1 |
2 |
0 |
1 |
1 |
1 |
Leg |
2 |
2 |
1 |
1-2 |
1-2 |
1-2 |
Foot |
3 |
3 |
2 |
3 |
2 |
2 |
The test with the tunic fork we change.
We use of course a towel for restriction of the vision but most patients don’t know what the must feel, therefore we have change the procedure. The sensation of the tunic fork isn’t by many people familiar, therefore people don’t know what the must feel.
Therefore we test first with vision the tuning fork against the bone of the jaw. Be careful because this can be a heavy sensation. After that we test the tuning fork on the bone part of the first toe, malleolus and under leg till the bone structure of the knee. It was remarkable that so many people with the disease dementia feel clearly the tuning fork vibration at the bone structures of the knee. That means that the gnostic sense (the translation of that what we see of the quality of the floor- slippery etc.) isn’t there.
-Perception assessment start from the first moment when a person going to lie in neither bed nor the bench. Is he lying straight or oblique and can he correct this without vision control is very important. We know that people with decreasing cognitive lie often oblique and that is in their perception is straight [56]. We know that is also the case when they stand or walk [57] but there is so much more. And the tuning fork vibration give us the certainly that the gnostic sense isn’t good anymore.
-Test about feeling where the arms or legs are in the air isn’t also less (mirroring-body position) but especially by hand [58] and feet often the information is very low as we search for feeling in general but also for movement under the foot (discrimination sense) and that means that fall detention that must occur under the foot at first isn’t not there [59].
Perception, tone and movement are elements of the same brain control systems that we need for balance etc. By people with dementia this is very difficult to get good in the picture and see how important these elements are also for the daily movements.
Par example: we walk on a floor that looks slippery but how we control this? Through the gnostic sense and when that isn’t good anymore, than will everyone hold the feet on the floor to hold the best control. This does everyone when he walks on a floor that looks and is slippery. These elements tell us also how bad the perception is and that we must create an environment that gives extra attention for support elements as the railing in the corridor or by special places or corners.
Still there is observation that we could make and that tells us something about this perception local but also totals.
An few examples;
- Place people on the edge of a bed in sitting position with the under leg hanging down with no support under the feet. Everyone will start to move the feet and legs in a rhythm because the brain will know where the feet are. Is that connection poor we see that movement less or not.
- Lying on the back in bed, it is strange as people lay with the legs out each other. Normal we see after a while that the feet search each other but when this not happen is prepare that the perception is very poor.
- Place the hand of the person under the table and play under the table with objects to that person. Often you feel that people with the disease dementia are not capable that to do as we and every time look under the table or hold the hand back.
- What is the hand doing though the day? We know that normally especially the hand is almost always with each other or something busy. That is the input that the brain wants because that center want to know where the hand are. By person with neurological damage as dementia often the hand had a high tone and is close or people are continue busy with the hand and on “harder” manner and that are an indication that the brain has problems with the perception.
- Give people something in their hand and asked what that is par example a coin or soap.
- Walking without lifting the feet can be a sign of loss of perception.
- And the oblique lying attitude in bed.
Be sure that the quality of sense is good:
-Vision; -Hearing; -Taste; - Smell: Often in long care facilities very bad investigated and also very bad controlled [60].
Summary: Tone and perception - Mister C.
The connection between bad perception and higher tone is also by him clear. The perception look bad in the feet and legs and there is the tone at his highest. That makes balance for him a difficult thing and he can make no speed to correct some situations. His trunk has also a high tone but not clear or this is only paratonia or there is also an tone increase to get more control over the balance and walking. Tone increase of the neck and balance problems is well known and also more extension in the upper trunk with flexion increase in the elbow. Important is that we get clear what the balance possibilities are in relation with the tone and perception but also in relation with strength and coordination possibilities. Bad coordination will be a part of an increase tone but still this coordination can be treated and help to decrease the tone.
Test from the lower trunk in sitting position, can give clearness of the possibilities of the trunk to participate in the total balance strategy. In sit the sideways balance reaction with crossing leg is important because that tell us or there are possibilities in the rotation muscles in the hip. In sit to front and back is often not value because people will search to fast for support and then it is no balance reaction.
In stand we assessed the balance with ‘statiek “- technique [64, 65]. This technique gives on pelvic and shoulder height a little pressure and assesses the reaction. Is that reaction on time and equal on the pressure that is given? Further we look or the ankle and hip/trunk strategy is appropriate. In front and back this two must be acted together and must give the feeling that the pressure against the body feels as a wooden board. No movement and a reaction that is equal with the pressure and ready for when the pressure is gone.
This test asked for feeling because the reaction can be so different and the sensitivity of the test is great. When someone is good trained he can feel of the legs and feel that there is an difference of leg length.
Balance reactions Sit - Sideway
To the left |
Head |
Goes to the left ( no elongation) |
|
Trunk |
Stay in an shortening position. |
|
Trunk start |
Trunk makes first an upper trunk sideways to the left ( shortening) |
|
Left arm |
Is not total free from the chest of the therapist (picture 1) |
|
Right arm |
Of the bench |
|
Left leg |
Exorotation present but passive |
|
Right leg |
Is over the left leg but clamp it and that means that so the base is created. |
To the right |
Head |
Goes to the right. |
|
Trunk |
Stay in an shortening position. |
|
Trunk start |
Trunk makes first an upper trunk sideways to the left ( shortening) |
|
Left arm |
Is not total free from the chest of the therapist |
|
Right arm |
Of the bench |
|
Left leg |
Exorotation present but passive |
|
Right leg |
Is over the left leg but with support of the therapist. |
Remarks: An active independent Exorotation isn’t possible on both sides. Further when he sit on his buttock he “Fall” down. That is a sign that the tone of the buttock isn’t increase, on the contrary the tone of the muscles is decreasing and also the control and coordination.
Balance reaction in standing position (test by static technique) Mister C.
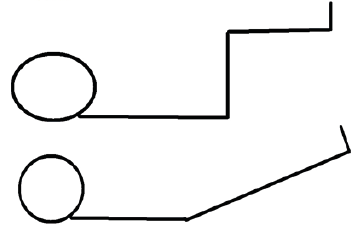
Resistance on hip – and shoulder height. (Examples of the statiek technique figure 2 and 3):
Picture 2 Picture 3
Forward therefore a pull on hip – shoulder height
Remarks: The answer of him on pull was late and the first time he steps to the front. After 3 times he was capable to react good on hip-height, but at shoulder height he must every time give some flexion in the hip before he could brace the pull and react on the pull?
Reaction of the left foot. |
Plantar flexion is present but late and not total, only the heel comes from the floor. |
Reaction of the right foot. |
Idem |
Reaction lower trunk left. |
On shoulder level there was every time a movement before the muscle of the trunk and hip were capable to brace the pull. There was no active extension in hip and trunk through the 0 degree hip, thus no complete balance reaction as on picture 3 and 6. |
Reaction lower trunk right. |
Idem. |
Step right |
When he wasn’t able to hold the pull, than there must a high against-reaction [66] and an shift to left leg and an step to the front. That was very difficult and mostly he places his hand on the shoulder of the therapist and makes an step. |
Step left |
Almost the same. |
Remarks: Power plantar flexors both side to low. Test stand on leg and push the body high with the heel-foot sole free and that 10 time fast. He gets only the heel good of the floor and those only 5 times and then decreases the lift very fast.
The reaction of the trunk was by every test the same.
Backward therefore push on hip- shoulder height. (Picture 2 and 3)
Reaction of the left foot. |
Dorsal flexion is there immediately. |
Reaction of the right foot. |
Dorsal flexion is there immediately |
Reaction lower trunk left. |
The reaction on the pressure was deleted. The foot reaction was there but he needed more time to build up the pressure against the push. This was on pelvis height so, also on shoulder height and there was the time he needed longer. |
Reaction lower trunk right. |
Idem.7 |
Step right |
The brace possibilities were insufficient and that give him not enough time to place his weight on the other foot and place his foot backward. The reaction of the trunk was often also late and that make an fast placing of the free foot difficult [66] |
Step left. |
Idem |
Remarks: The power of the dorsal flexors was lower than normal. Fixation of the forefoot by a movement of the whole body to the back was poor. Is this power or a sign of increase tone by greater speed?
Side way left . Pressure left, and pay attention that he stay on left leg.
Reaction of the left foot. |
No reaction was visible. That isn’t necessary because the first reaction must occur on hip level. A fast reaction in the foot is an sign that there is an problem. |
Reaction lower trunk left. |
The reaction was late and not done by the left leg but trough the right leg. Never was he able to block the pressure immediately. |
Step right |
Because the trunk makes no elongation was the right foot not capable to cross over but makes abduction. |
Side way right. Pressure right and pay attention that he stays on the right leg. (Hip-shoulder)
Reaction of the right foot. |
No reaction was visible. That isn’t necessary because the first reaction must occur on hip level. A fast reaction in the foot is a sign that there is a problem. |
Reaction lower trunk right. |
The reaction was late and not done by the left leg but trough the right leg. Never was he able to block the pressure immediately. |
Step left. |
Because the trunk makes no elongation was the right foot not capable to cross over but makes abduction. |
Remarks: Sideway must they block immediately because that we create an elongation out the lower trunk. When the hip is passed the lateral edge of the foot we see a foot reaction and can there be a crossing of the free leg.
The free leg- movements are dependent of the trunk movement:
Trunk forward- free leg backward. Trunk backward – free leg forward. Trunk elongation– free leg abduction. Trunk shortening – free leg adduction.
Mister C. has thus a great problem with a good reaction of the trunk /hip movement and therefore free leg movement and with good placement on one leg.
The one leg standing test was 3 sec, together with this statiek test tell us that he stand by the one leg standing test with an upper trunk sideway and cannot control one leg standing.
Summary balance: the balance is poor and he cannot control balance shift independent. He needs an extra support point. This because he isn’t capable to brace the fall movement so well that he create a foot free and can use a step-strategy with success.
In supine position look not only to the trunk but also the shoulders, hands, legs and foot on the right and the left side. Through the supine situation is the influence of a pathological tone less because less frees movement and less influence of the gravity. Still make the movements not too fast and look of there are elements of pathological synergy.
Pre -test of the tone of the stomach; Place your fingers around the ribcage left and right, asked the person to relaxed and try to go so far as possible. When you feel resistance asked the person to lift his head and feel the tension return or let him laugh. Normal is that there is room for 1-2 cm.
By Mister C. Were this almost 5 cm and the tension occur slow. The test by mister C. further:
Left leg lift.
The arms on the stomach was not possible, he needed the support of the edge of the bench.
The right leg makes an end rotation that goes too far, but was stopped through him with using his arm especially his left hand/arm.
Resistance on the left leg was minimal and the plantar flexion increase and his arm/hand work hard.
The pressure under his right buttock was low and not the whole muscle was activated. The pressure under the heel was low but the plantar flexion was huge.
Pressure against the left leg to lateral of medial; He could a little pressure controlled but the most was done with his arms. His right foot stay in the same position makes not more rotation but the heel stay not on the same place.
Remarks: The plantar flexion increase and the lack of controlled rotation in the hip gives an indication that the pathological tone is in this attitude so great that control of the right leg is poor.
To be sure we do the tentacle test:

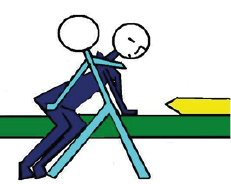
Picture 4. This example shows the tentacle test with the arms in the air but of course they may on the stomach or at the edge of the bench. Even support is allow (on the leg that stand on the bench) but realize that that he use that support to use the pathological synergy /tone.
Tentacle of the right leg and lift the left leg
Mister C. could lift the buttock in the air and could lift than the left leg. But the height of the buttock lift was fast decreasing and he must use his both arms to control the hip rotation. After a few seconds his right leg was slipping in extension.
Remarks: No optimal hip/lower trunk control in the extension and rotation part. Further clear signs that there was an increasing use of the pathological synergy /tone were necessary to get this job done.
Lift of the right legs gave the same results: Thus on both sides was control of this movement without the pathological synergy/tone not possible. Control of this movements asked therefore very much of his upper trunk and head and he use therefore much upper trunk backwards as part of the back diagonals. The result that we say in the balance test in sit and stand is here present.
Summary Diagonals: The power and the coordination in the lower trunk and hip /Leg is poor and there are clear symptoms of pathological synergy and tone.
Which obstruction you have found also hyper mobility?
Head: In the cervical spine there are especially on the right side mobility loss in the joints. This asked for a special treatment [67].
Arm; The right shoulder suffer from a part. Rupture of a tendon (M. Supraspinatus) and asked for an special treatment and echo-assessment [68].
Investigation according Butler. Nerve tissues [69-71].
1. General: Head and trunk (Slump); Slump is difficult and on the right side more than the left side. This pointed on a lumbar problem or pressure on the nerve tissue. In his history is a hernia on the right side. He has now no complaints but his mobility is lesser
2. Arms: The nerve tissue test of the left arm is good, but on the right side is the mobility of the n. median us and n. ulnar is lesser. Here is a treatment with slide movements necessary and that can have also a positive influence on the shoulder.
3. Legs: The right n. ischiadicus (lacquer- test) is lesser than the other side. The mobility is lesser and then there is also some pain. Slide techniques are indicated.
Summary alignment: There are some problems that asked for extra investigation and specialized treatment but this is necessary because pain has a negative influence on tone and also on balance [72].
MRC= Movement Resistance active
0 = no contraction to feel.
1 = Visual and palpable contraction.
1, 5 = Movement possible without gravity force.
2 = Movement over the whole tract without gravity force.
2, 5 = Partial movement against the gravity force.
3 = Movement against the gravity force over the whole tract.
3, 5 = Movement against light resistance over the whole tract.
4 = Movement against reasonable resistance.
4, 5 = Movement against strong resistance but still not normal.
5 = Normal muscle force
|
Movement |
Resistance |
|
Movement |
Resistance |
Head |
Flexion |
3 |
Elbow |
Flexion |
Left Right
4 4 |
|
Extension |
4, 5 |
|
Extension |
4 3 |
|
Lateral. left |
4, 5 |
|
Supination |
4 3 |
|
Lateral. right |
4 |
|
Pronation |
4 4 |
|
Rotate left |
4, 5 |
Wrist |
Ulnar deviation |
4 4 |
|
Rotate right |
4 |
|
Radial deviation |
4 4 |
Trunk Sit |
|
|
|
Dorsal flexion |
4 4 |
Upper |
Flexion |
3 |
|
Palmar flexion |
4 4 |
|
Extension |
4 |
Fingers |
Flexion |
4 3, 5 |
Whole trunk |
Rotate left |
4 |
|
Extension |
4 3, 5 |
Whole trunk |
rotate right |
3,5 |
Thumb |
Extension |
4 4 |
Lower |
Flexion |
3 |
|
Flexion |
4 3, 5 |
|
Extension |
4 |
|
Opposition |
4 3, 5 |
Whole trunk |
Lateral. left |
4 |
|
Abduction |
4 4 |
Whole trunk |
Lateral fl. right |
4 |
|
Adduction |
4 4 |
Arm |
|
|
Hip |
Flexion |
3 3 |
Shoulder blade in side lying |
Elevation |
Left Right
4 3 |
|
Extension |
3 3 |
|
Depressive |
4 4 |
|
Abduction |
2,5 2,5 |
|
Laterorot. |
4 4 |
|
Adduction |
4 4 |
|
Mediator. |
5 5 |
|
Endorotation |
3 3 |
|
Adduction |
5 5 |
|
Exorotation |
3 3 |
|
Abduction |
4 3 |
Knee |
Flexion |
4 4 |
Shoulder |
Anteflexion |
4 3 |
|
Extension |
3 3 |
|
Retroflexion |
4 3 |
Ankle |
Dorsal flexion |
2,5 2,5 |
|
Abduction |
4 3 |
|
Plantair flexion |
3 3 |
|
Adduction |
5 4 |
|
Inversion |
3 3 |
|
Exorotation |
4 3 |
|
Eversion |
3 3 |
|
Endorotation |
4 3 |
Toe |
Flexion |
4 4 |
|
|
|
|
Extension |
3 3 |
Summary active resistance: This investigation has an amount of subjectivity that is the reason that the 5 isn’t reached. But still this fact is that the power of the muscles in the leg is low, too low. Is this the influence of the pathological tone or is it possible that there is also an great amount of atrophic and Sarcopenia [76, 77] When we compare his performance on the Senior fitness Test [29] than there is an base to think that he has to little power and coordination. That make a treatment with task specific resistance treatment possible but we must confirm that treatment with the presence of the pathological tone/synergy.
Cognition etc.
Modified observation list of Dr. Berna Rood [75]
Attention
Disturbances in arousal and concentration
Disturbances in pointing and selective attention.
Disturbances in partial attention.
Disturbances in flexibility of the attention and changing of attention area.
Disturbances in constraint attention.
Extinction
Tactile agnosia
Somato-agnosia
Spatial agnosia
Intentional apraxia
Ideatoir apraxia
Memory
Disturbed short memory.
Disturbances in the appealing of information from the long memory.
Orientation
Orientation in time.
Orientation in place.
Orientation in space
Communication
Written communication
Executive functions
Disturbed disease insight
Loss of initiative.
Planning and organization
Flexibility
Impulsiveness
Disturbed self-control and self-correction.
(Think on Tone, Active /passive, diagonals, perception balance and alignment).
The power and the coordination of the lower trunk and hip/leg are of a low level. There are clear elements of a pathological tone and the synergy in the legs are present. Alignment problems are present but not so prominent that this has a devised effect. The power and the tone are the greatest problems and make it for him too heavy to functioning as he want.
The balance is poor because when he is out of the balance he isn’t able to correct this only with support of arms/hand but not with a balance reactions from his whole body.
Speed a pathological tone is the greatest problems and it will be difficult improvements to realize. But when we can control the tone and increase the power and the coordination than there are possibilities to counter the loss of independency and improve his quality of life.
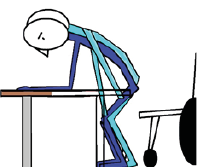
Immediately: The treatment must start as soon as possible but the power and tone are still the same? But the strategy that is done now, give no reason to go one. This will give an reaction of all people that are involved but the assessment give an clear answer that the way that is treated give no improvement. Still the discussion was heavy because the therapist was offended but again the assessment was clear. Now it was clear that he has no assessment and couldn’t give a reason why he wasn’t capable to come out his bed and walk to toilet. The only therapy he give was standing up and walking through the corridor 3 times a week and there were no data what he has improve or loss. Be honest, there are in long care or nursing home even by elderly therapist that will act on the same way and that isn’t therapy.
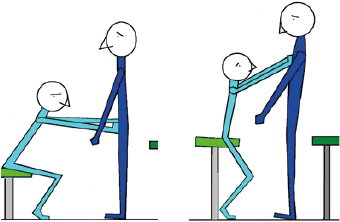
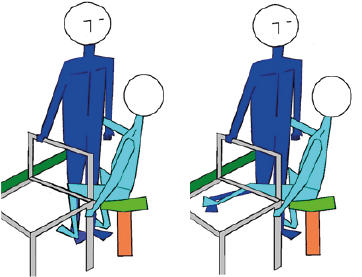
1. The environment makes things difficult. The training that he must stand up by using the arms on the chair support and then grasped the rollator frame was doomed to fail and that was on this moment to heavy. Never underestimated the heaviness of ADL- movement and that the whole day, therefore we search immediately to a way that is less difficult. Therefore on the head-end of the bed we place a table that he can use to stand up from the bed. The bed- fence makes the placing of the feet difficult and painful and therefore we remove it. The toilet was the other difficult item, see the photos 6. An the solution (photo 7) to support the standing up was also created by the bed and was introduced in the transfer training that now start on the ward by the therapist 3 times an week and nurses after an instruction. (Photo 8)

Picture 6 Picture 7
Photo 6 and 7. Photo 13 is situation that was for Mister C. present but that was no option because he couldn’t make in this situation the standing up and had no support when he stand and correct his clothes. We search for an alternative and we found the toilet on photo 14 and now he grasped the washbasin and make an good Vorlage with an perfect foot placement and had an support when he stand. This created a situation that there was an possibility to train his ADL.

Photo 8. The technique show on photo 5 as the advantage that the movement to the front is complete and that will give a good foot placement. When he grasped the edge of the table with the elbow supported on it, he pulls himself further to the front and that gives more body weight to the front and makes the extension of the leg easier. And of course the situation is safe!!
The technique that he use, we trained before on the physical ward (photo 5).
By placing a table on the head edge of the bed he could use the same technique when he get to stand out of the bed.
2. After the improvement of the environment, it is important that the training take place there were he needed it. That means that the therapist exercises on the ward in movements in bed, coming to sit on the edge, standing up with the table and walk to the toilet. Undressing and sit and after that standing up and take care and dress himself. But that is only 3 days, the other days must be done by the nurses and we introduced and instruction program for the nurse show to do it and how to facilitate the movement when he cannot do it. This facilitation program is a part of the training to get the movement done on the way he must do it but give also the assistance that he needed. On such an way he use the possibilities that he had and he hope that as we get him stronger that he take over. The base was formed out :
- turning in bed.
- coming to sit on the edge
- standing up and sitting done with the support on the front. More about this transfer technique in Chapter 4.
Turning in bed –facilitation
Picture 5. Turning in bed asked for a push with the leg that is on far side and with an active lift of the upper trunk.
The push with the leg asked for extension and will turn the lower trunk to the other side and the lift of the head and the upper trunk follow that movement. To facilitate this is one hand needed on the “far” leg and a lift assistance of the upper trunk also on the fare side.
Picture 5 gives a start model but it is important that the legs are less in flexion because extension in the legs makes control to the side lying better possible through the action of the hip in the foot. The heaviness of this movement is high but because the movement is done on bed the gravity isn’t so big and will the tone not fast increase. Important to realize that the end of the turn when some is coming to side lying, asked for a control though the foot and arms.
Coming to sit on the edge of the bed
Picture 6. Facilitation of this movement asked for a fixation of the lower trunk. By placing the working hand on the upper leg this fixation is there and now the person can use his possibilities optimal. The hand by the shoulder is mostly not necessary but controlled the movement of the upper trunk in the correct plane.
Standing up behind an table
Picture 7. Technique is support on the elbow and pulls the body to the front over the table. Facilitation can the best be given through a movement of the upper trunk to the front by a light push against the shoulder and by a push on the upper leg to stimulated the extension in the knee. Picture 10 -11 are more against the gravity and will evoke a higher tone. Therefore be sure that movement is done with not too much speed.
This three technique are be done by Mister C. by the therapist and the nursing staff on the ward through the whole day and especially at night when he goes to the toilet. The advantage of this approach is that everyone can do it but can also give the differences on the diver’s moment through the day and night. That there was a difference was clear but at night, he has more problems to start because his tone was lower than through the day. Sleep decrease his tone and power and he need more time to resort his tone.
This is very important because this create a problem extra. The tone was decrease when he sleeps and must move and is our treatment poor enough to increase that tone at night without increasing the pathological tone!!
3. Specific treatment of muscle pattern to increase the power and the coordination of the lower trunk/hip without an increase of the pathological tone. The amount of power that is lacking is great and is especially needed by the movements in and out bed. Standing up is the heaviest movement against the gravity but it is no too early to train on an improvement of the balance in stand. Therefore we choose for a treatment in supine and side-lying position. In supine position we can train on the push with far-side leg with a load that is 75% of 1 R.M [74] and that 3 sessions of 10 and we look or we feel and see muscle fatigue. This program 3 times a week will improve the power and the coordination of the movement [78-80]. The tentacle can be done also but we know that he cannot do it with load and he cannot push his buttocks very high because the pathological synergy will make control impossible. Therefore we choose for a little lift and an little lift of one leg and then change. Side lying position is than the next step and here we have extra coordination training and that is balance control.

Picture 8. Give an impression of an start with the legs in flexion and lift the leg that lies above. The leg that lies under must work and control and with load we can reach a 1.R.M.of 75 % and create more power and coordination.
Picture 9. An impression how heavy this side lying exercise can be. In this case without load but the amount of control in the hip and shoulder on the bench is huge. The abductors of the hip must contract concentric and with endo-and exorotation in the hip.
4. The last treatment part was hydrotherapy. Here we can work on a decrease of the tone and the pathological synergy and create more speed and coordination in the movements. We place an chair in the water and when he sit on that the water level was somewhat under shoulder level and train him to get standing up without hand support but in the beginning with facilitation.
Lying in the water and try to turn to the side with facilitation was another part of the treatment [81-83] and with assistance of another person we started with a task specific resistance treatment for the legs with the most emphasis on the standing phase but in supine position.
One hand is on the front of the ankle and braces the flexion of that leg, but to lift this leg the other leg must make extension and create an anchor. Therefore the other hand is under the heel and that is the most important hand. There we train the muscle pattern that he needed in the stand phase. On photo 17 the amount of resistance is far too much!!
Of course we exercise also the walking abilities in the water with increasing of the speed that will give resistance through the water.
After 2 Months
On the ward the nurses give after 1 month that the amount of facilitation was almost zero. Only at night there were occasions that he needed the facilitation but that weren’t every night. Furthermore he was through the day capable with supervision to go alone to the toilet but needed assistance with his clothes.
At night the wasn’t always the case but there were night he was capable to do it with supervision but needed assistance with his clothes. This was the moment that a training to get this done be started through the occupational therapy and their advises for the night.
The environment had everyone convinced, thus we hold this changes.
The exercises were going good and the load can be change to a higher level and in the pool he started with balance training in standing position. More information in Chapter 4.
On land we started now with the balance- and walking training but also with task-specific resistance treatment for both.
The lower trunk/hip muscles and coordination was the weakest part of his body. The pathological tone/synergy makes training in stand difficult because of the increase use of this pathological tone and synergy. Therefore we choose for training in water to decrease the tone and make movement with more speed possible.
Furthermore fall training on land by Mister C. isn’t feasible, because of the speed that is necessary for the correct execution but in water he can exercises the fall without great risk. But the translation of this on land will never be taken place. Some elements will be taken over as the brake possibilities with the feet and the trunk/hip but that asked for more power and coordination in lower trunk/ hip and that part can be exercised on land. Therefore we must carry for a situation will good support that decrease the tone /synergy.
Picture 10 Picture 11
Picture 10 and 11. Resistance against the free leg to treat the standing leg. That can be done for the abduction muscles but also for the extension muscles and the variation for the rotation is also possible. The resistance against the free leg must be answer by the standing leg and when that is too little the swing cannot be making. Through the fixation by the chair and therapist the tone is controlled. The resistance started by 60% of 1 R.M. but increased
That this was possible created a situation that he restored his ability to get out the bed and go to toilet after 3 months and he was complete independent.
The conclusion was therefore that he was working under his possibilities and that the treatment he received was insufficient. Furthermore the environment in which he must function was not adequate and makes things difficult.
But we will also with this program, reach his limits and then it will be difficult to hold him on this level. This because the illness progress and therefore also his pathological tone and synergy and it is thus important the level of the exercises adapt. Hydrotherapy will be an essential part for this treatment and give him as long as possible the possibilities to move independent.
Still after 3 months this result is great and means that it is important to assess everyone and make a good treatment plane instead of walking with a rollator frame.
A good assessment will show where the greatest problems are and gives a treatment plane a base. A when there is no progression than is often the best way to do the assessment another time and search further.
Mister C. moves on level below his possibilities and her receive no adequate treatment, but when the was clear that the lower trunk/hip has suffer of an pathological tone but also of an loss of muscle power and coordination that wasn’t see and treat.
This people deserve the same treatment that others get.
- Ramakers I.,Visser PJ., Aalten P., Boesten. J., Metsemakers J., et al (2007) Symptoms of Preclinical Dementia in General Practice up to Five Years before Dementia Diagnosis. Dementia and Geriatric Cognitive Disorders.
- Mirelman A., Maidan J., Bernad H., Shustack S., Giladi N., et al (2017) Effects of aging on prefrontal brain activation during challenging walking conditions. Brainb and Cognition.
- Van de Rakt J., McCarthy- Grunwald S (2020) Dementia, How We Can Created the Best Quality of Life for Them 1-20.
- Van de Rakt J., McCarthy-Grunwal., d S. Elderly (2018) Normal senso-motoric performance. Part 2 Muscle reaction on the restriction of the trunk. In progress.
- Van de Rakt J., McCarthy-Grunwald S (2020) Physical treatment of individuals with dementia. Part 1 A. Italian Journal of Sports rehabilitation and Posturology 7: 1546 -1581.
- Van de Rakt J., McCarthy-Grunwald S (2021) Physical treatment of individuals with dementia. Part 1B. Assessment- WHY. Italian Journal of Sports rehabilitation and Posturology 16: 1694-1730
- Van de Rakt J., McCarthy-Grunwald S (2019) Physical treatment by individuals with dementia. Exercises Phase 4 (Rakt-scheme) for individuals with dementia. Italian Journal of Sports rehabilitation and Posturology. 9: 2054 -2091.
- Kraft P., Gadeholt O., Wieser M., Jennings J., Classen J (2009) Lying obliquely-a clinical sign of cognitive impairment: cross sectional observational study. BMJ 336: bs273.
- Robinovitch S., Feldman F., Yang Y., Schonnop R., Luen P., et al. (2012) Video Capture of the Circumstances of falls in elderly people residing in in long-term care :an observational study. The lancet 5: 381.
- Van Schooten K (2014) Predicting falls. Amount and quality of daily-life gait as risk factors. Thesis 30-78
- Burnfield J (2012) Kinematic and electromyographic analyses of normal and device-assisted sit-to-stand transfers. Gait & Posture 36: 516-522.
- Van de Rakt J., McCarthy-Grunwald J (2017) Diagonals Part Five-Pathology How can we develop the diagonals so each individual achieves optimal recovery following a stroke? Italian Journal of Sports rehabilitation and Posturology 4:746 -788.
- Duysens J (2015) Differences in foot sensitivity and plantar pressure between healthy young and elderly. Arch Gerontol Geriatr. 63: 67-71.
- V.d.Plaats A., De Boer G (2013) Het demente brein. Breincollectief 25-46.
- Van der Plaats A (2008) De wondere wereld van dementie. Elsevier.
- Geelen R., Van Dam H (2016) Dementie: van hersenlagen to omgangsvragen. BSL.
- Nilgun Kuru Alici., Pinar Zorba Bahceli., Oya Nuran Emiroglu (2018) The preliminary effects of laugther therapy on loneliness and death anxiety among older adults living in nursing homes: A non-Randomised pilot study. Int J Older People Nurs.13: e12206.
- Alici N and others (2020) Effects of laughter therapy on life satisfaction and loneliness in older adults living in nursing homes in Turkey. Rehabilitation nursing.00.1-9.
- McCarthy- Grunwald S (2019) Send in the clown: The humour paradox in dementia. Presentatio.
- Van de Rakt J., McCarthy- Grunwald S (2019) Dementia Part One: A Physical Treatment of Individuals with Dementia. Journal of Dementia 2: 107.
- Donker Kaat L., Boon A., Heutink P., en Van Swieten J (2004) Progressieve supranucleaire verlamming; een bijzondere vorm van parkinsonisme. NTvG 148: 519-523.
- Van de Rakt J (2018) The Environment in Long-Care Facilities (Nursing Home) Decrease the Possibilities to Move Independent! Global Journal of Research and Review 5:10
- S. Fenn K (2016) Sleep Less, Think Worse: The Effect of Sleep Deprivation on Working Memory. Journal of Applied Research in Memory and Cognition 5: 463-469.
- FiField K (2017) Does Sleep Apnea Lead to Alzheimer’s? AARP.
- Mirelman A., Hillel I., Rochester L., Del Din S., Bloem B., et al. (2020)Tossing and Turning in Bed: Nocturnal Movements in Parkinson’s Disease Movement Disorders.
- Van de Rakt J (2021) Observatie-formulier Vervolgcursus Psycho Geriatrie.
- Koolstra M.Burgers I., Lemmens J., et al. (2001) Klinimetrie na een beroerte. NPI/VU Medisch centrum.
- Schädler S., Kool J., Lüthi H., et al. (2006) Assessments in der Neurorehabilitation UItg. Huber.
- R. Rikli., C. Jones (2002) Senior Fitness Test. The Journal on Active Aging 1-30.
- Collin C Wade D (1990) Assessing motor impairment after stroke: a pilot reliability study. Journal of Neurology Neurosurg Psychiatry 53: 576-579.
- 31.Demir Y., Aksu S (2014) Reliability and validity of Trunk Control Test in patients with neuromuscular diseases. Physiotherapy Theory and Practice 3: 1-6.
- Holden M.K. et al., (1984) Clinical gait assessment in the neurological impaired: Reliability and meaningfulness. Physical Therapy: 64: 35-40
- Mahoney F. Barthel D (1965) functional Evaluation: The Barthel Index. Maryland State Med Journal 14: 61-65.
- Hyndman D Ashburn A. (1995) Stops walking when talking” as a predictor of falls in people with stroke living in the community. BMJ 311:83-86.
- Collen F.M., Wade DT., Bradshaw C.M (1990) Mobility after stroke: Reliability of measures of impairment en disability. International Disability Studies12: 6-9.
- 36.Van Eijk M (2012) Predicting prosthetic use in elderly patients after major lower limb amputation. March 2. Prosthetics & Orthotics International 36: 45-52
- Collin C Wade D (1990) Assessing motor impairment after stroke: a pilot reliability study. J Neurology Neurosurg Psychiatry 53: 576-579.
- Schoene D., Wu SM., Mikolaizak AS., Menant JC., Smith ST., et al. (2013) Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis.
- Van de Rakt j (2021) Omgeving remt zelfstandigheid. Tijdschrift voor verzorgenden. In progress.
- van de Rakt J., McMarthy-Grunwald S (2021) Elderly “normal” senso-motoric performance. Part 1.
- Van de Rakt J., McCarthy-Grunwald S (2018) Diagonals Part six. Standing up and the static reaction. Italian Journal of Sports rehabilitation and Posturology 5: 926-989.
- Zwakhalen S (2004) Dutch version (translation) by the University of Maastricht.
- Jorik Nonnekes., Evzen Ruzicka., Tereza Serranova., Stephen G. Reich., Bastiaan R. Bloem.,et al. (2020) Functionele gait disorders A sign-based approach.. Neurology 94:1-7.
- Carr, J., Shepherd R (1980) Physiotherapy in disorders of the brain. London: William Heineman.
- Davies P (1999) The comprehensive treatment of patients with hemiplegie. Second edition. Completely revised and updated. Springer-Verlag.
- Barnes M.Johnson G (2001) Upper motor neurone syndrome and spasticity Uitgever. Cambrigde University Press.
- Bohannon R.W., Smith M.B (1987) Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys.Ther 67: 206-207
- Waardenburg H. en anderen (1999) Is paratonie betrouwbaar te meten? Ned.Tijdsch.v.Fysio. nummer 2
- Tardieu G., Rondont O., Mensch J., Dalloz J., Monfraix C., et al. (1997) Responses electromyograhpiques a l’etirement musculaire chez l’homme normal. Revue Neurologie 60-61.
- Hobbelen J. Paratonia enlightened (2010) Defenition, diagnosis, course, riskfactors, and treatment. Proefschrift. Enschede, Gildeprintdrukkerijen, Maastricht University 143.
- Hobbelen J and others (2006) Paratonia: a Delphi procedure for consensus definition. J Geriatr Phys Ther 29: 50-56.
- Haugh, A. B., Pandyan, A. D., & Johnson, G. R (2006) A systematic review of the Tardieu Scale for the measurement of spasticity. Disability and Rehabilitation 28: 899-907.
- Van de Rakt J., McCarthy-Grunwald S (2020) Treatment possibilities of “contractures “by neurological diseases. Ita. J. Sports Reh. Po 7: 1450 -1478.
- Akeson W., Amiel D., Mechanic G., Woo S., Harwood F., et al. (1977) Collagen cross-linking alterations in joint contractures: changes in the reducible cross-links in periarticular connective tissue collagen after nine weeks of immobilization. Connect Tissue Res 5: 15-9.
- Drenth, H., Hobbelen, J., Zuidema, S. U., Bautmans, I (2020) The role of inflammaging and advanced glycation end products on paratonia in patients with dementia. Experimental Gerontology 142.
- Kraft P., Gadeholt O., Wieser M. Jennings J., Classen J (2009) Lying obliquely-a clinical sign of cognitive impairment: cross sectional observational study. BMJ: 336: bs273.
- Robinovitch S., Feldman F., Yijian Yang Y., Schonnop R,. Ming Luen P., et al. (2013) Video Capture of The Circumstances of fallas in enderly people residing in long term care: an observation study. Lancet 381: 47–54.
- Van Deun B., Van Den Noortgate N., Van Bladel A., Palmans C., Cambier D (2018) The Impact of Paratonia on Fine and Gross Motor Function in Older Adults With Mild and Moderate Dementia. Alzheimer Dis Assoc Disord.
- Le Goic M., Wang D., Chiarovano E., Lecompte J., Laporte S., et al. (2018) An Initial Passive Phase That Limits the Time to Recover and Emphasizes the Role of Proprioceptive Information. Frontiers in Neurology.
- Riemersma-van der Lek RF., Swaab DF., Twisk J., Hol EM, Hoogendijk WJ, et al. (2008) Effect of bright light and melatonin on cognitive and non-cognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA.
- Van de Rakt J., McCarthy-Grunwald S (2018) Diagonals Part 7 Stroke 5 Walking: What say the scientist and what is best practice. Ita. J. Sports Reh. Po 5: 1013-1062.
- Van de Rakt J., McCarthy-Grunwald S (2019) Diagonals Part 8. Stroke 6 Analysis of walking pattern and treatment. Ita. J. Sports Reh. Po 6:1191-1238.
- Van de Rakt J., McCarthy-Grunwald S (2019) Diagonals Part 9 Analysis of walking pattern. Learn to assess. Ita. J. Sports Reh. Po 6: 1253 -1294.
- Worm G (2011) Cursus waarnemen en behandelen. Papendal.
- Van de Rakt (2018) Statiek. Nieuwsbrief . NHV.
- Van de Rakt J (2013) Balanstraining bij ouderen. Physios 3: 12-24.
- Mulligan B.R (1995) Manual Therapy; Plane Vieuw Services, Wellington, New Zealand. Ottenheijm RP., Vant Klooster IG., Starmans LM., Vanderdood K., De Bie RA., et al. (2014) Ultrasound-diagnosed disorders in shoulder patients in daily general practice: a retrospective observational study. BMC Fam Pract 15: 115.
- Butler DS (2000) The sensitive nervous system. NOI Publications, Adelaide Australia.
- Butler D.S (1991) Mobilisation of the nervous system. Churchill Livingstone.
- Shacklock M. Clinical (2005) Neurodynamics. Elsevier Butterworth& Heineman.
- Mirelman A., Maidan I., Bernad H., Shustack., S Giladi., (2017) Effects of aging on prefrontal brain activation during challenging walking conditions. Brainb and Cognition 41-46.
- R.J.O. van der Ploeg en H.J.G.H. Oosterhuis (2001) Fysische diagnostiek - het meten van spierkracht.N.T.v.G.
- Branten J en anderen (2021) De verhouding tussen de 1RM en 10 RM waarde in een populatie kwetsbare ouderen in een verpleeghuis. NTvGF 25: 31-40. Rood B (2006) Cognitie in het dagelijks leven van de CVA –patiënt. Thesis 24-101.
- Bautmans I., Vantieghem S., Gorus E., Lauwers E., FIERENS Y., et al. (2021) Age-related differences in muscle recruitment and reaction-time performance, from Proceedings of the 2nd International Conference on Sarcopenia Research (ICSR) meeting. The Journal of Frailty & Aging 1: 207.
- Vandewoude M., Bautmans I (2009) Prevention (of Sarcopenia): is it possible? Sarcopenia, eds.
- Bosch F (2010) Krachttraining en coördinatie. Uitgevers 30-56.
- Hettinger T (1983) Isometrische muskel training Georg Thieme Verlag Stuttgart.
- Lieber R.L (2002) Skeletal Muscle structure, function, plasticity Lippincott Williams & Wilkins.
- Lambeck J( 2001) Hydrotherapie. Uigave N.P.I.
- Van de Rakt J., McCarthy-Grunwald S (2019) Physical treatment (Hydrotherapy) by individuals with and without dementia. Aquatic exercising. Part 1 ta. J. Sports Reh. Po 9: 1989-2017.
- Van de Rakt J., McCarthy-Grunwald S (2021) Physical treatment (Hydrotherapy) by individuals with and without dementia. Aquatic exercising.