Endometrial stromal uterine sarcoma is distinguished by a high degree of malignancy. There is an aggressive course of the disease, as a result of which additional tumor nodes may appear, both in nearby organs and in distant organs (metastases). The cause of death in about 90% of cancer patients is not a tumor, but a metastasis. Endometrial stromal uterine sarcoma is characterized by a rather unfavorable prognosis with a high degree of hematogenous localization, as a result of which the sarcoma spreads through blood vessels to all human organs. The number of mitosis for an enlarged microscope is greater than 10 out of 10 fields of view. Endometrial uterine sarcoma is observed in women aged 45-50 years. The diagnosis is most often made after the histological analysis of the operating room. The classic treatment is abdominal hysterectomy with bilateral appendectomy.
Uterine sarcomas are a heterogeneous group of high-malignancy cancers that develop from the uterine body. Common manifestations include abnormal uterine bleeding and pelvic pain or mass. We report the case of a 70-year-old patient, widow, mother of a child, postmenopausal 12 years ago, followed for high-grade invasive ductal breast carcinoma, luminal B Her2 positive dating back to 11 years, admitted for postmenopausal menometrorrhagia. Ultrasound and MRI revealed a globose uterus measuring 8.8 cm, thickened endometrium measured at 10mm, then the patient underwent biopsy endometrial curettage, the results were in favor of high-grade endometrial stromal sarcoma. The patient underwent a total hysterectomy with bilateral appendectomy. The histological study with immunohistochemical complement concluded that there was high-grade endometrial stromal sarcoma with hormone receptor negative.
Through this rare case, we insist on the epidemiological, diagnostic, therapeutic and prognostic characteristics of this entity.
High-Grade Endometrial Stromal Sarcoma; Malignant Genital Pathologies; Endometrial Biopsy
Uterine sarcomas are rare tumors they represent less than 3% of malignant tumors of the female genital tract and 3 - 7% of malignant tumors of the uterine body.
Endometrial stromal sarcomas (ESS) have traditionally been classified into low-grade and high-grade types based on the level of mitotic activity [1].
A tumor originating from the stroma of the mucous membranes of the uterine walls. The course of this disease can be both aggressive and relatively benign, which is due to the biological characteristics of the neoplasm (parameters, genomic disorders, rate of progression).
Stromal uterine sarcoma of the endometrium, according to the most common version of specialists, develops from nascent stromal cells, or appears as a result of metaplasia of neoplastic cells. Such a tumor is clinically manifested by bloody discharge from the vagina, a two-handed study can reveal an increase in the size of the uterus, sometimes with a non-uniform consistency. High-grade endometrial stromal sarcomas (GESS) further infiltrate the myometrium and have a more aggressive course, with frequent metastases and poor prognosis. The studies of Norris and Taylor define the EHRES (Extrem High Risk Entertainment System) by the presence of more than 10 mitosis for 10 PBMCs (peripheral blood mononuclear cell).
We report the case of a 70-year-old patient, widow, mother of a child, postmenopausal 12 years ago, followed for high-grade invasive ductal breast carcinoma, luminal B Her2 positive dating back to 11 years, admitted for postmenopausal menometrorrhagia. Ultrasound and MRI revealed a globose uterus measuring 8.8 cm, thickened endometrium measured at 10mm, then the patient underwent biopsy endometrial curettage, the results were in favor of high-grade endometrial stromal sarcoma. The patient underwent a total hysterectomy with bilateral appendectomy.
We report the case of a 70-year-old patient, mother of a child, menopausal 12 years ago, with a history of conservative surgery on high-grade invasive ductal carcinoma, luminal B Her2 positive 11 years ago.
At the initial clinical examination: cervix of normal appearance with minimal endouterine bleeding, a pelvic ultrasound was done objectifying a globular uterus measuring 8.8 cm, thickened endometrium measured at 10mm, then the patient benefited from biopsy curettage of the endometrium, the results were in favor of a high-grade endometrial stromal sarcoma.
Immuno-staining:
Ac Anti-H-Caldesmone: negative
Ac anti-Pan-Cytokeratin: Negative
Ac Anti-CD10: Focal positivity of tumor cells.
Anti-ER ac: Negative on tumor cells.
Anti-Ki67 ac: Labeling estimated at 80% of tumor cells.
Ac anti-actin smooth muscle: Focal positivity of tumor cells.
Ac anti-WT1: Negative.
Ac anti-P53: Diffuse positivity of tumor cells.
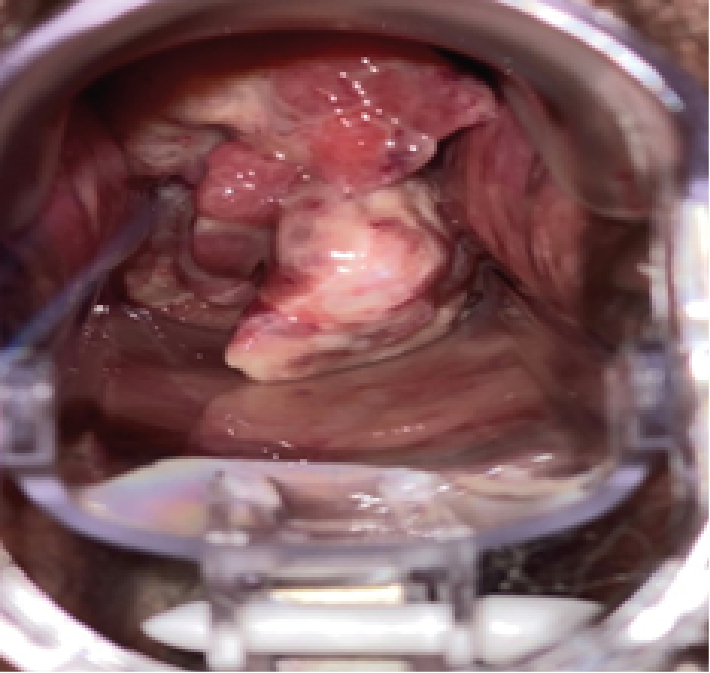
After biopsy curettage of the endometrium, there is a rapid clinical progression of the lesion on examination: presence of a budding lesion delivered by the cervix, bleeding on contact, free parameters (Figure 1, 2).
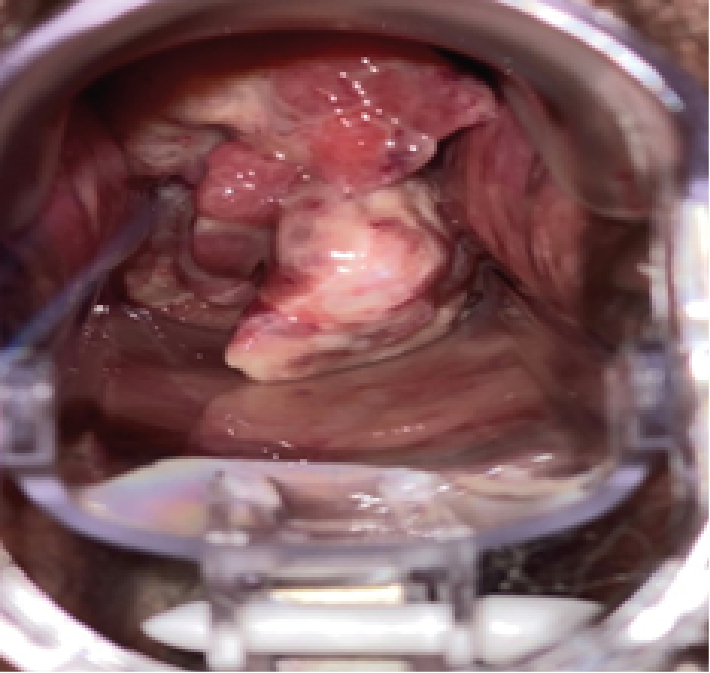
Figure 1: Budding lesion delivered by the cervix
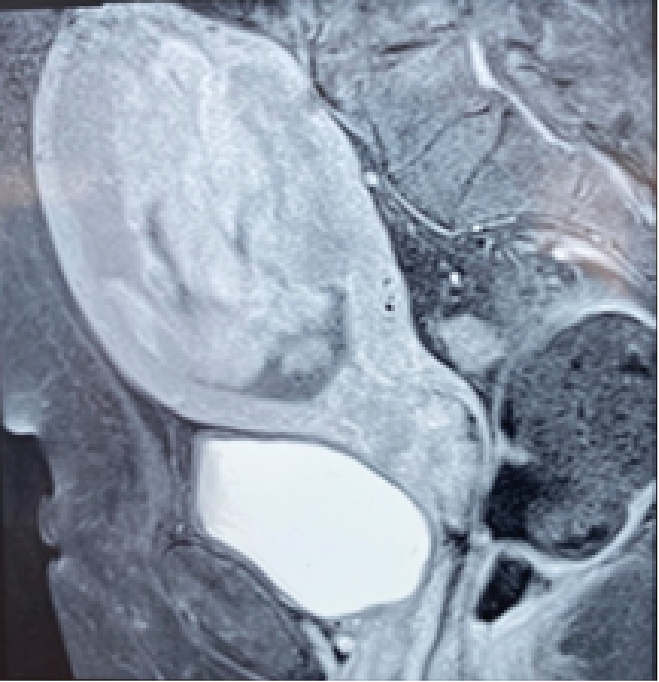
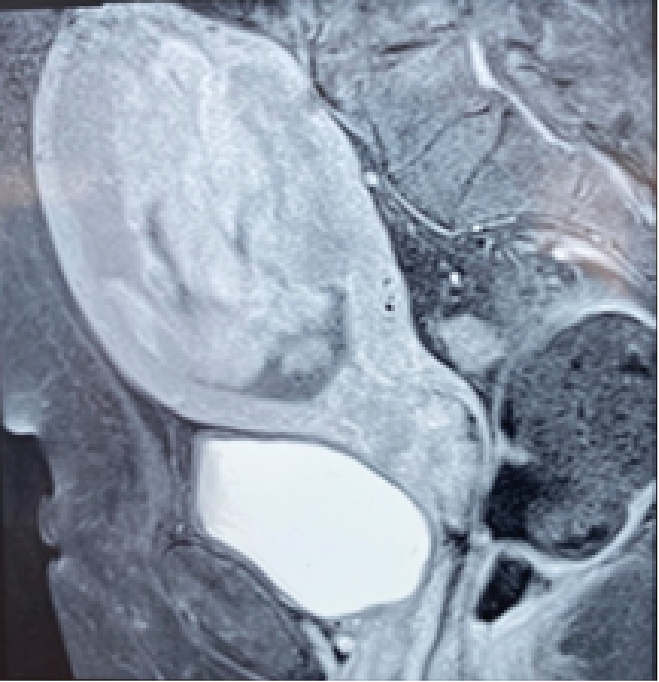
Figure 2: Pelvic MRI showing the lesion
Lumbo-pelvic MRI: Enlarged uterus in size, measuring 16 cm of major axis, seat of a well-limited endometrial process, irregular contours in places, delimiting areas of necrosis, measuring approximately 165x 105x 75 mm. This process laminates the myometrium especially in fundics. At the bottom, it passes through the cervical opening and extends to the upper third of the vagina. At the bottom and back, it invades the cervical myometrium and arrives at intimate contact with the anterior wall of the middle rectum with loss of the fatty border of separation in places.
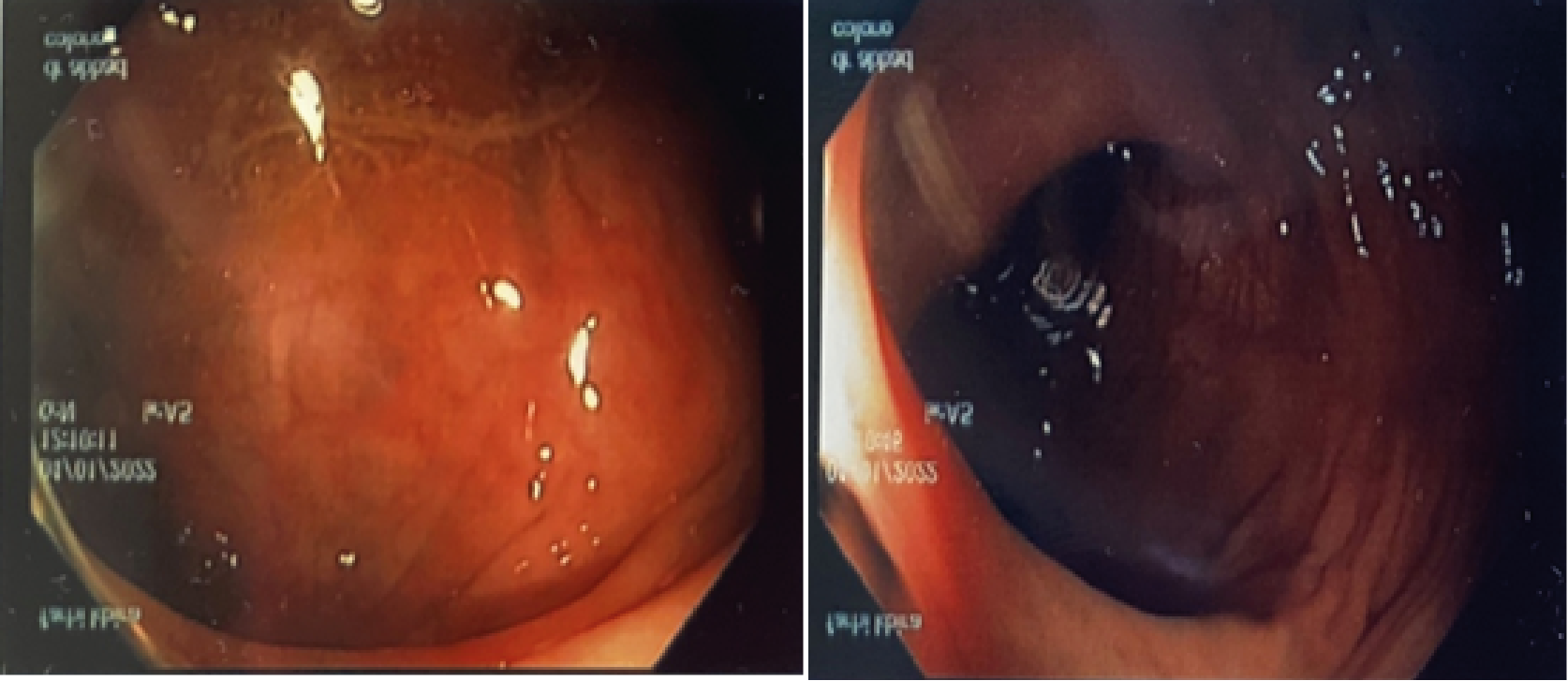
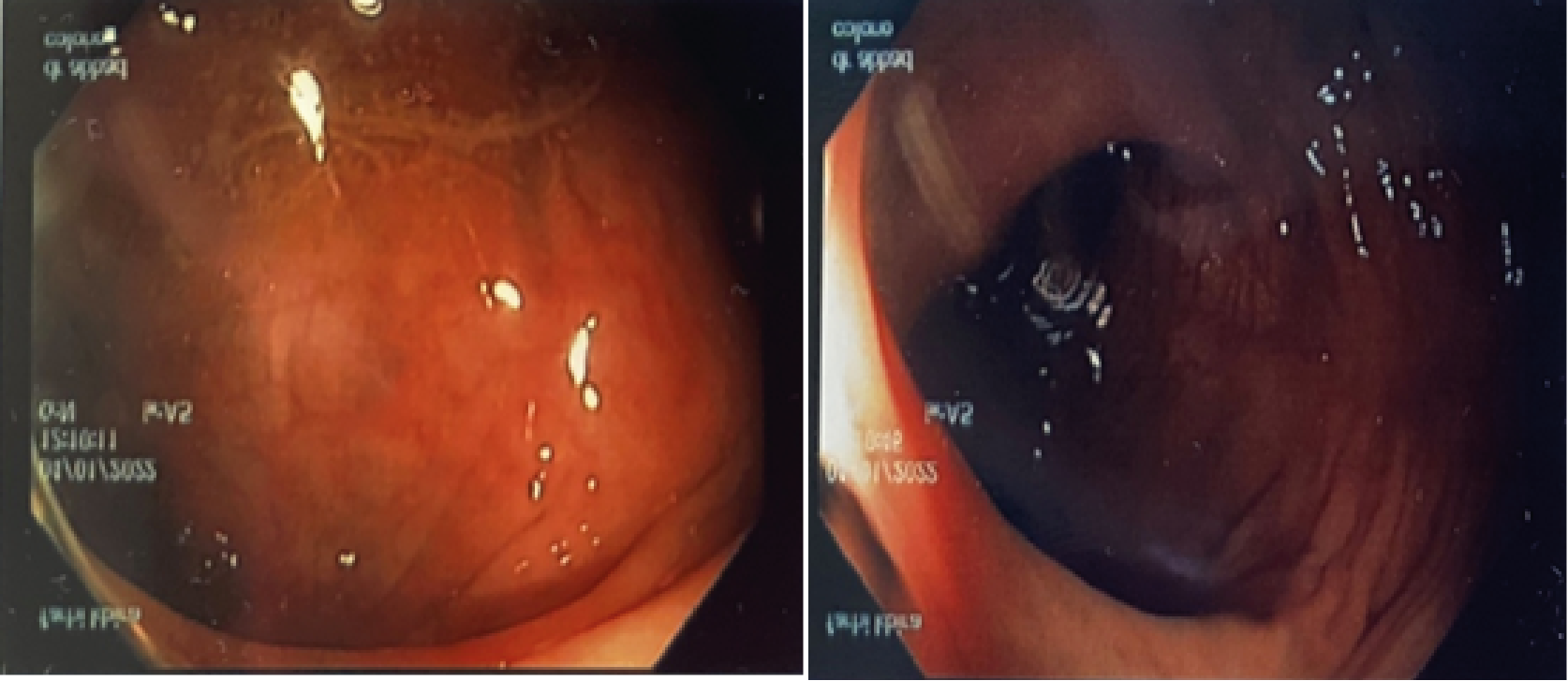
Figure 3: Recto-Sigmoidoscopie
Recto-sigmoidoscopy: Normal mucosa with the presence of some erythematous beaches, no presence of tumor, polyp or other lesions. (Figure 3).
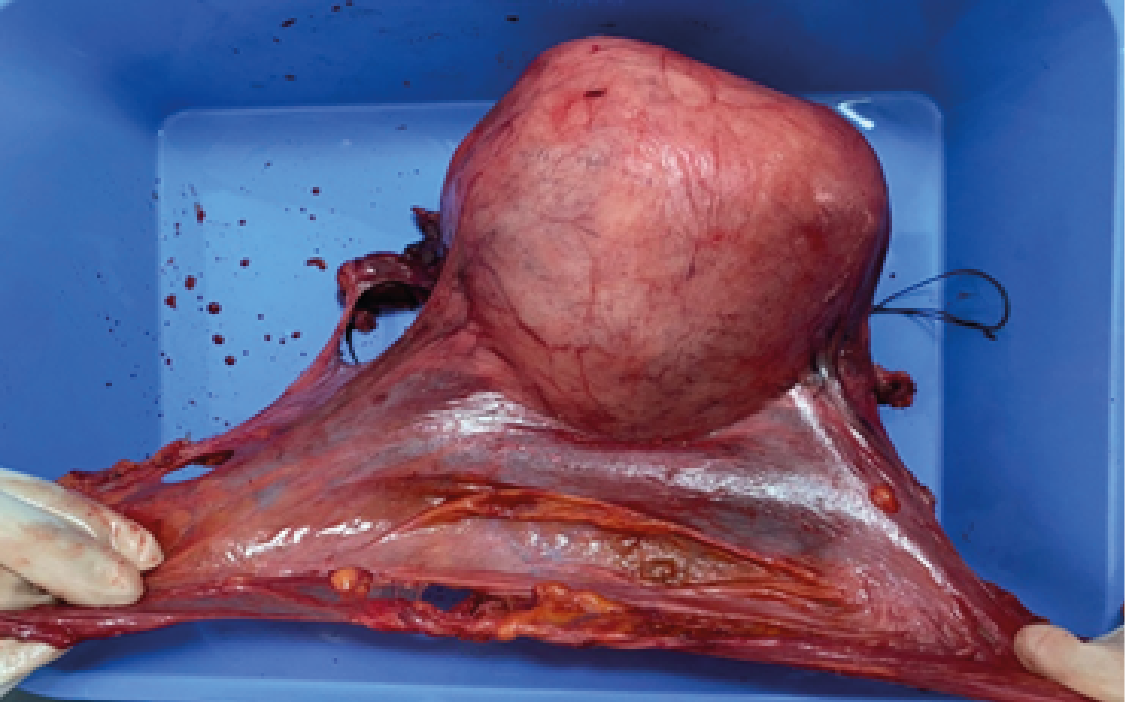
The patient underwent an enlarged total hysterectomy with bilateral appendectomy (Figure 4).
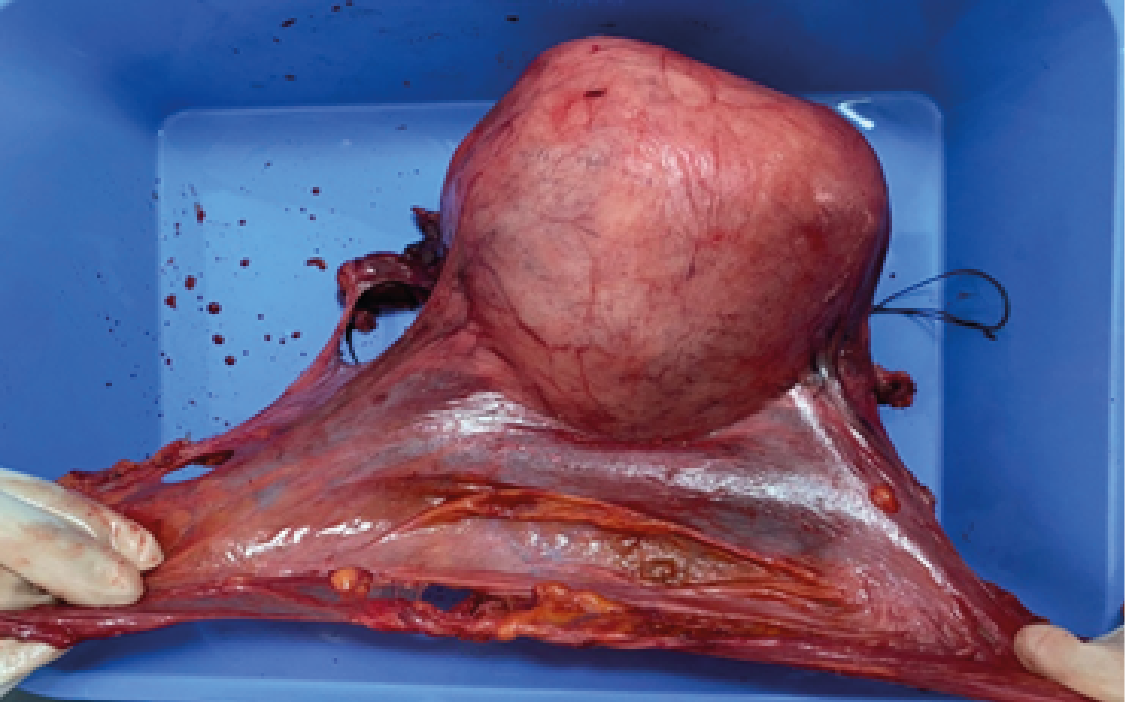
Figure 4: Hysterectomy room and appendices
Final anapath results:
High-grade endometrial stromal sarcoma
According to the National Cancer Database, which is a comprehensive, national, facility-based database established by the American Cancer Society and the Cancer Commission of the American College of Surgeons, survival for patients with HG-ESS remains low. Median overall survival is 19.9 months (95% CI: 17.1-22.1 months) and overall survival at five years is only 32.6% (95% CI: 30.1-35.3%). Endometrial stromal tumours are rare and make up less than 5% of uterine tumours [2]. They are composed of cells closely resembling the cells of the endometrial stroma in the proliferative phase. They are classified into two categories: stromal nodules, benign, and endometrial stromal sarcomas, including endometrial stromal sarcoma (low-grade) and undifferentiated endometrial sarcoma (formerly high-grade) [2, 3]. The stromal nodule is the least common endometrial stromal tumour [1]. It has the same morphological appearance and immunohistochemical profile (CD 10 expression) as low-grade endometrial sarcoma. The only histological element to distinguish the nodule from low-grade endometrial sarcoma is the absence of invasion of the myometrium and lymphatic and vascular structures [1, 3], which makes it necessary to perform a hysterectomy to determine the tumor margins [1]. Endometrial stromal tumors mainly affect postmenopausal women [4]. Their clinical manifestations are non-specific and are dominated by metrorrhagia and pelvic pain occurring. The diagnosis is most often made after the histological analysis of the operating room. In some cases, an endometrial biopsy will provide a diagnosis before surgery. The prognosis of these tumors is poor and patient survival is correlated with the tumor stage at the time of diagnosis [5].
There are many methods for treating uterine sarcoma, but the most common can be considered a surgical method followed by chemoradiation. Surgical treatment allows you to first determine the stage of the disease with the subsequent removal of the main part of the tumor. This method of treatment is used at an early stage of the disease. In other cases, when the disease is detected late, surgery is not enough. Other methods of treatment are needed here. When it comes to radiation therapy, it is one of the most effective ways to treat uterine sarcoma today. It should be noted that surgical treatment or chemotherapy alone will not give positive results. This method of treatment "works" only in a complex. The combination of these two treatment methods allows you to get rid of the roots of the tumor, and consists of a total hysterectomy with bilateral appendectomy by laparotomy to avoid possible fragmentation of the tumor related to vaginal excision [6].
In case of low-grade endometrial stromal sarcoma, a bilateral appendectomy is recommended because of the hormonal sensitivity of these tumors, however, in case of high-grade undifferentiated sarcoma, bilateral appendectomy has not demonstrated its interest [6]. In the absence of macroscopic involvement, it is not systematic in premenopausal women. When histological diagnosis is made postoperatively, reintervention can be discussed (totalization of a subtotal hysterectomy, appendectomy) in advanced forms, broad surgery must be discussed according to imaging arguments in case of metastatic recurrence, surgery of metastases should be discussed [6]. For endometrial stromal sacomas: radiotherapy has not shown interest in poorly differentiated sarcomas: pelvic radiotherapy (50 Gy in 25 fractions without brachytherapy) may reduce pelvic recurrence but does not increase overall survival [7].
It is optional, to be discussed according to the risks of toxicity, radiotherapy may be proposed when the excision is incomplete due to the extension of the disease. When surgery is contraindicated or refused by the patient, exclusive radiation therapy may also be discussed [7]. Medical treatments: in an adjunct situation Adjuvant chemotherapy has not yet shown any clear benefit. In the metastatic phase, chemotherapy has shown its interest even if overall survival remains low. Depending on the different molecules used, response rates vary between 17 and 42% [6]. For high-grade endometrial stromal sarcomas, the chemotherapy regimens mainly used include ifosfamide. In low-grade endometrial stromal sarcomas, many relapses but few die. Several studies report sometimes long responses with hormone therapies with medroxyprogesterone acetate, megestrol acetate [8]. Antiaromatases and LHRH analogues were also tested. Tamoxifen is contraindicated. HRT is also contraindicated after treatment.
Poor prognostic factors associated with survival include patient age, tumour size, missed lymphadenectomy, pathologically positive margins of resection, and distant or lymph node metastases. Some of these poor prognostic factors were noted in our patient, including large tumor size and metastases to the peritoneum and pelvic lymph nodes.
In the case of a high-grade malignancy, the woman only has to undergo supportive treatment and fight the disease until the last moment, however, low-grade ESS is a disease that has a fairly good prognosis. If the pathology is diagnosed in time and therapy is started, the survival rate is more than 5 years. Endometrial stromal tumors are rare tumors of the uterus that mainly affect postmenopausal women. The symptomatology of endometrial stromal tumors is nonspecific. In addition, these tumors have a great histological diversity the diagnosis is based on morphological, immunohistochemical or even molecular biology criteria.
Conflicts of Interest
The authors state that there is no conflict of interest regarding the publication of this article and Written informed consent was obtained from the patient for the publication of this case report.
- Sarcoma of the uterus, Cancer (oncology).
- Bal A., Mohan H., Aulakh R., Huria A (2008) Endometrial stromal lesions: a morphological and immunohistochemical study of short series. Arch Gynecol Obstet 277: 21-24. [Crossref]
- Prat J (2009) FIGO staging for uterine sarcomas. Int J Gynecol Obstet 104: 177-178. [Crossref]
- Brown L (2008) Pathology of uterine malignancies. Clin Oncol 20: 433-447. [Crossref]
- Leung F., Terzibachian JJ., Aouar Z., Govyadovskiy A., Lassabe C (2008) Uterine sarcomas: clinical aspects and Histopathological. About 15 cases. Gynecol Obstet Fertil 36: 628-635. [Crossref]
- Reed NS (2008) The management of uterine sarcoma. Clin Oncol 20: 470-478. [Crossref]
- Stadsvold JL., Molpus KL., Baker JJ., Michael K., Remmenga SW (2005) Conservative management of a myxoid endometrial stromal sarcoma in a 16-year-old nulliparous woman. Gynecol Oncol 99: 243-245. [Crossref]
- Taïeb S., Narducci F., Chevalier A., Baranzelli MC., Ceugnart L., et al. (2008) Imaging of uterine sarcomas. Imaging of the Woman 18: 229-235.
- Szklaruk J., Tamm EP., Choi H., Varavithya V (2003) MR imaging of common and uncommon large pelvic masses. Radiographics 23: 403-424. [Crossref]