Background: Patient safety is an undeniable important aspect in the context of improving the quality of the entire health system. Improving patient’s safety should be comprehensive and include two dimensions of safety – technical and functional. One source of information about the level of patient’s safety are medical staff, but there is a gap here, which is no central system that would collect, analyze and draw conclusions from a sufficiently large number of problems reported by stakeholders.
Objectives. The aim of this study was to evaluate the patient’s safety on the basis of the declaration of nurses.
Material and Methods: The study involved 160 professionally active nurses. The study was performed by the authors questionnaire based on the questionnaire “Hospital Survey on Patient Safety Culture” developed by the Agency for Healthcare Research and Quality. The selection of the sample was based on the availability of respondents. The study was performed in January 2021. More than ¾ of respondents indicated the hospital as a place of employment.
Results: Nearly 40% of respondents said that their boss rarely and very rarely takes into account the suggestions of employees for the improvement of patient’s safety. Over 40% of respondents said that their workplace is often and very often trying to do too many tasks and too fast.
Conclusions: It is necessary to create a culture of safety by improving communication between doctors and nurses or line manager and nurses. There is a need for greater involvement of line manager in solving problems reported by nurses in terms of providing safe care to patients (Piel. Zdr. Publ. 2021, 5, 1, 33–39).
Nurse; Interpersonal Communication; Patient’s Safety; Health Care Quality; Adverse Event
Patient safety is an important aspect in the context of quality improvement in the entire health care system, especially in the area of hospitals, where the effects of adverse events are likely to pose a greater threat to the health and life of the patient than in outpatient care [1].
Improving patient safety must be comprehensive. To this end, it should cover two dimensions of security - technical and functional. The technical dimension understood as professionalism of operation. It concerns such components of safety as education, practical skills, experience of medical workers, the number of medical personnel adjusted to the state of health and the number of patients, sanitary and hygienic conditions in which patients are staying, conditions for storing medicines, technical condition of medical apparatus and equipment.
However, ensuring safety in this dimension does not guarantee that the patient will not be harmed. It is equally important to ensure safety in the functional dimension, which is understood as the professionalism of the relationship. This dimension relates to broadly understood communication with the patient and may include such components as: comprehensible transfer of information, showing empathy and understanding, devoting time and attention to the patient or asking about their needs. Taking these two dimensions into account in the management of the risk of adverse events provides the basis for achieving a significant improvement in this particular case of the quality of patient safety [2, 3].
Difficulties in managing the above-mentioned area of quality, however, are caused by the lack of reliable information on meeting the criteria of the technical and functional dimension, which is particularly important in the case of medical entities providing services such as “hospital 24-hour health services”. While in the case of medical entities that have obtained accreditation from the Center for Quality Monitoring in Healthcare in Krakow, it is possible to assess the fulfillment of the above-mentioned criteria more closely, in the case of other medical facilities it is not feasible [4].
One of the sources of information about the degree of fulfillment of the above criteria are the medical workers themselves, but there is a gap here - the lack of a central system that could collect, analyze and draw conclusions from a sufficiently large group of problems reported by medical personnel and / or patients [5].
The study was designed to collect and evaluate information on patient safety based on declarations by professionally active nurses.
The study included 160 nurses who declared employment as a nurse in a medical entity. The study was conducted using the proprietary questionnaire based on several questions regarding the content of the questionnaire "Hospital Survey on Patient Safety Culture" developed by the Healthcare Research and Quality Agency - AHRQ. Occasional sampling was used. Only descriptive statistics were used to analyze the results. In order to obtain 160 questionnaires, 200 questionnaires were distributed (sample implementation rate - 80%). The survey was conducted in January 2021.
More than three-quarters of respondents indicated the hospital as a workplace. The length of service in the profession in months was as follows: ≤ 12 - 54%,> 12 and ≤ 36 - 16%),> 36 - 14%, the missing data constituted 16%.
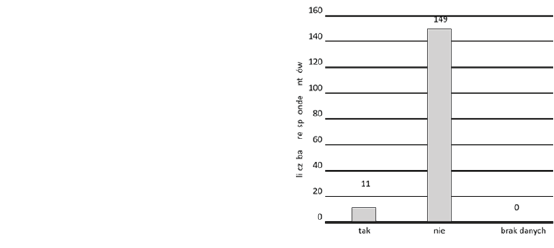
Almost a quarter of the surveyed nurses made a mistake in administering pharmacotherapy to their patients during their work (Fig. 1). Given that the question uses the term "ever", it seems that the scale of adverse events reported by nurses in this popular type of therapy is relatively small. However, it should be noted that the length of service in the profession of respondents in half of the cases did not exceed a year.

Figure 1. Have you ever given a patient the wrong medicine, or the wrong dose of medicine, or a medicine that he should not get, whether the error was due to nursing or medical intervention? (n = 160)
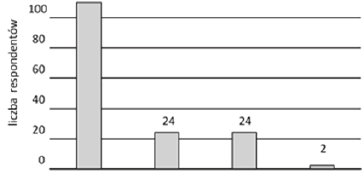
The general scale of adverse events (Fig. 2) in the place of employment of the surveyed nurses (it should be remembered that these are subjective declarations) indicates that these events are sporadic (answer: very rare and rarely - 84%).
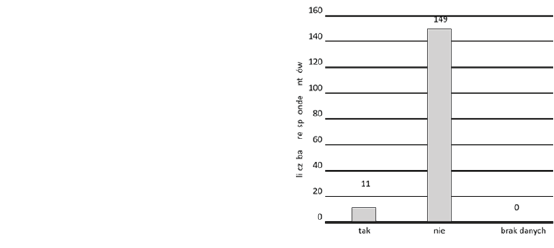
Figure 2. Please indicate how often the following errors (wrong drug, wrong patient, wrong dose, etc.) made by nurses and physicians happen in your workplace (n=160)
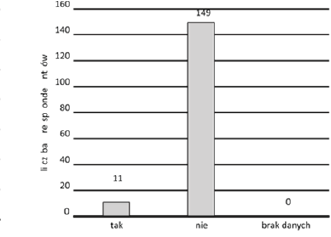
Most of the surveyed nurses are convinced that information about adverse events occurring in their workplace is not available to them (answer: very rare and rarely - 65%). On the other hand, the literature [6] indicates that an effective way to reduce the severity of adverse events is the implementation of Reporting and Learning Systems (RLS). This system is based on the principle of transparency of the mistakes made for other members of the organization, thanks to which it is possible to develop solutions aimed at their elimination. Based on the respondents' declarations (Fig. 3), it can be assumed that such a system does not work in the medical units of the surveyed nurses - it poses a greater threat to hospitalized patients than if such a system existed.
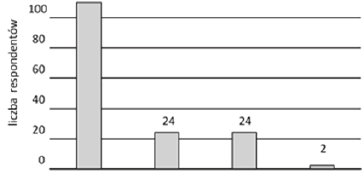
Figure 3. Are you informed about errors made by nurses and physicians that happen in your workplace (n=160)
Declarations of the surveyed nurses regarding the storage of drugs in their workplace raise serious doubts as to the safety of patients in the field of pharmacotherapy. The responses of about one third of the respondents suggest that the patients received drugs which, due to the temperature at which they are stored, do not guarantee their suitability for treatment (answer: no - 15%) or that the storage conditions are not controlled (answer: I do not know - 15%), so it cannot be guaranteed that these drugs do not endanger the health of the patient (Fig. 4).
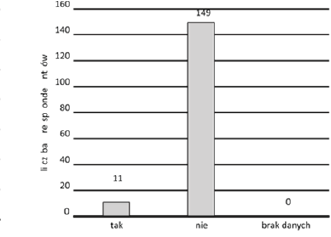
Figure 4. In your workplace. Are drugs always kept in conditions that ensure the temperature recommended by the manufacturer, e.g. below 25°C? Take into account the summer seasons (n=160)
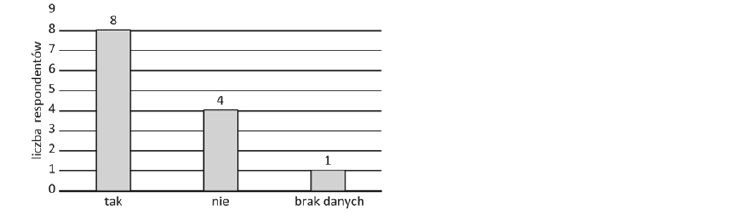
An important issue from the point of view of patient safety is the psychophysical efficiency of medical personnel. In the case of multiple employment in the Polish health care system [7], the question arises whether the person caring for the patient, eg a nurse, is psychophysically fit. The collected data show that only 7% of nurses declare second employment (Fig. 5).
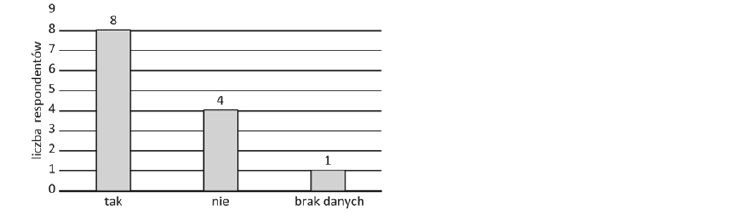
Figure 5. Do you sometimes have to go to work on a day shift after a night shift? (n=13)
It should be noted, however, that the respondents are also students, which may have a significant impact on the decision not to take up additional employment. This is especially dangerous for the patient when the shift nurse moves to the next workplace after a night shift. It is equally dangerous for both the nurse and the patient (Fig. 6).
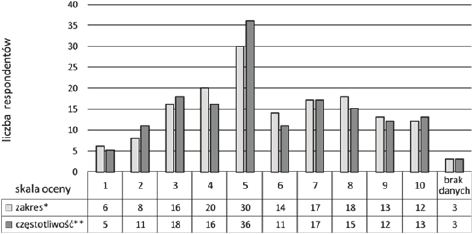
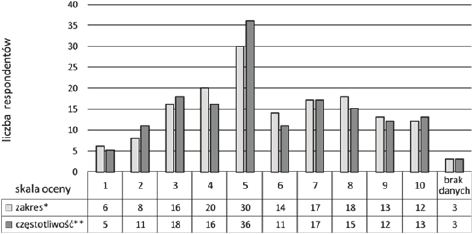
Figure 6. How do you assess the scope and frequency of information exchanged with physicians about the current state of a patient? Select the table with a cross (where “0” is a low score, and “10” high score) (n=160)
In terms of patient safety, communication between people caring for the patient (eg a nurse and a doctor) [8]. It seems that the more frequent the communication between the performers of the therapeutic process (quantitative approach) and the more details about the patient (qualitative approach), the more complete the picture of the patient's health status for individual members of the therapeutic team - appropriate actions to be taken at the right time. The collected data show that nurses are not satisfied with the frequency and scope of the exchange of information about the patient with the doctor, as half of the respondents assess these two parameters below the average (Fig. 7). Lack of communication adequate to the needs of nurses may significantly hinder the correct nursing diagnosis, and thus be associated with too late diagnosis and implementation of the necessary measures for patient safety.
Effective communication between the doctor and the patient can significantly reduce the stress associated with hospitalization [9]. Additionally, a patient who is inadequately informed about his or her health condition, planned therapy or prognosis cannot consciously decide about himself in the context of health and disease, which prevents the patient from participating in the treatment process based on the principle of partnership. The collected data show that the doctor-patient communication is ineffective (perhaps the information is not conveyed or is conveyed in a way that is incomprehensible to the patient), because the messages that should be conveyed by the doctor are usually (often and very often) communicated by the patient %) to be recovered from the nurse.
The collected data show that communication between members of the nursing team is satisfactory (answer: often and very often - 72%) for nurses even in a crisis situation, i.e. characterized by a large number of tasks to be performed in a relatively short time.
The workload of medical personnel is an important factor determining patient safety [10], both in terms of providing medical care on time and the time needed for proper observation / nursing / medical diagnosis. The collected data show that the organization of work in a significant (answer: often and very often - 44%) part of the jobs of the surveyed nurses is inappropriate. That is, the state of health and the number of patients is inadequate to the number of nursing staff.
A report from the Institute of Medicine (IOM, USA 2019) indicates that the most common cause of medical errors today is not carelessness, lack of knowledge or practical skills. The reasons can be found in the poor organization of the health care system [11]. The manager, instead of focusing his actions solely on punishing the employee, should first of all analyze the undesirable events in terms of ergonomic conditions and assess the degree of employee participation in the occurrence of an undesirable event - this approach is considered the most appropriate [11]. The collected data show that managers in the workplaces of the surveyed nurses lack such awareness (answer: sometimes, often, very often - 43%). This approach of the managers of the surveyed nurses is not conducive to solving problems related to patient safety.
As mentioned at the beginning of the work, medical personnel are an important source of information on adverse events. The comments made by medical personnel may significantly improve patient safety, reducing the number of situations favorable to the occurrence of both actual and potential harm to a patient [12]. The collected data show that the heads of the surveyed nurses to a large extent (answer: very rarely, rarely, sometimes - 66%) do not use the potential of the staff as a source of information on improving patient safety.
In the context of patient safety, it should be remembered that not only the error learning system (RLS) [6] is important, but also the system of continuing professional development (CPD) for healthcare workers. Scientific research confirms that the level of education affects the quality of care and the incidence of adverse events [13]. The collected data show that nurses' managers do not take sufficient measures to improve patient safety in terms of CPD (answer: very rarely and rarely - 51%).
The conducted research clearly confirms the need to improve patient safety in medical entities (in Poland) being the place of employment of the surveyed nurses.
Important conditions for increasing the safety of patients hospitalized in Polish hospitals include:
- Creating conditions that guarantee proper storage of medicines and developing mechanisms to control these conditions.
- Improving communication between management staff - nurses, doctors - nurses, doctors – patients.
- Motivating the immediate superiors of nurses to get involved in improving the work organization of their employees.
- Adaptation of the nursing staff to the health condition and number of patients, so that work does not have to be carried out in "crisis mode".
- Establishment of an anonymous system for reporting events affecting patient safety (RLS) in the hospital.
- Management efforts to increase the number of nurses involved in the process of continuous professional development (CPD), in particular through forms of education enabling the assessment of their results (ending with a knowledge and / or skills examination).
- Labon M (2003) Dangerous Hospitals. Health Manager.
- Czerw A., Religioni U., Olejniczak D (2021) Methods of measuring and assessing the quality of services provided in healthcare entities. Probl. Hig. Epidemiol 93: 269-273.
- Miller M., Supranowicz P., Gębska-Kuczerowska A., Car J (2018) Assessment of the quality of medical services by hospital patients. Epidemiol 62: 643-650.
- Lewandowski R (2012) Tools of quality improvement in health care. Entrepreneurship and management 8: 47-61.
- Kruk-Kupiec G (2022) Management of the risk of adverse events. Safe medical practice design. Document available from the website of the Ministry of Health.
- Gajewski P., Bała M (2021) Adverse events as part of the assessment of the quality of medical care in the hospital accreditation program. Med. Prakt.
- Golinowska S., Kocot E., Sowa A (2021) Human resources for the health sector. Current trends and forecasts. Zdr. Publ. Management 11: 135-136.
- Center for Postgraduate Education of Nurses and Midwives, Interpersonal Communication in Nursing (No. 09/17).
- Joumard I., André C., Nicq C (2019) Health Care Systems Efficiency and Institutions. OECD Economics Department Working Paper. OECD 769.
- Kirkman-Liff B.L., van der Ven W.P (2017) Improving Efficiency in the Dutch Health Care System: Current Innovations and Future Options. Health Policy 13.
- Lighter D.E (2018) Advanced Performance Improvement in Health Care. Principles and Methods. Jones and Bartlett Publ.
- Loeb JM (2014) The Current State of Performance Measurement in Health Care. International Journal for Quality in Health Care 16.
- Swayne L.E., Duncan W.J (2018) Ginter M.P Strategic Management of Health Care Organizations.