Introduction: Right hemi-diaphragmatic stimulation is a rare complication of dual chamber pacemaker. We report a case of 55 year old male who developed sudden onset right hemi-diaphragmatic contractions after 5 weeks of dual chamber pacemaker implantation.
Case Summary: A 55 years old male with a dual chamber pacemaker implanted for complete heart block presented with persistent uncomfortable rhythmic contractions of the right hemi-diaphragm five weeks after. Device interrogation suggested atrial lead dislodgement and fluoroscopy confirmed atrial lead dislodged into the superior vena cava. Diaphragmatic rhythmic contractions stopped when device was reprogrammed to VVI mode. Atrial lead was removed and replaced with a new lead. No rhythmic contractions of the right hemi-diaphragm were observed after reprogramming the device mode to DDD.
Conclusion: If diaphragmatic twitching is as a result of atrial pacing in a dual chamber device, reprogramming of the pacemaker mode to VVI will stop the diaphragmatic twitching.
Atrial Lead Dislodgement; Right Hemi Diaphragm Twitching; Diaphragmatic Contraction; Pacemaker; Phrenic Nerve
Right hemi-diaphragmatic twitching is a rare complication of dual chamber pacemaker [1]. It may require fluoroscopy, Chest-X-ray and interrogation for confirmation [2]. It may indicate indirect stimulation of the diaphragm (right-sided) through the right phrenic nerve. Apart from perforation, displacement of the atrial or ventricular lead could stimulate the phrenic nerve to cause diaphragmatic stimulation [1]. In the upper chest, the right phrenic nerve lies lateral to the right brachiocephalic vein and the superior vena cava (SVC) [3].
Depending on the lead which is responsible, the approach may include chest-X-ray or fluoroscopy, change of pacing mode and repositioning of displaced lead. Here we report a patient with diaphragmatic stimulation due to atrial lead displacement to the SVC who underwent re-operation and lead repositioning.
Case Summary
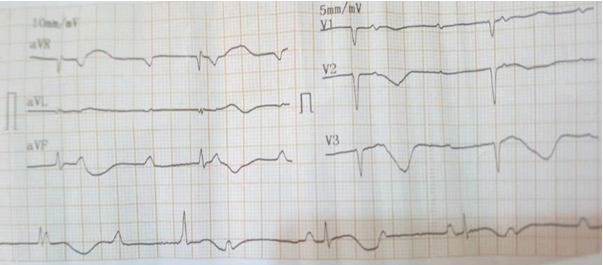
A 55 years old male non-diabetic and non-hypertensive with a 2 weeks history of dizziness and pre-syncopal attack. No history of palpitation, no chest pain and no syncopal attack. At presentation, he was not in obvious distress, afebrile, anicteric, no leg oedema. Pulse was 28bpm, blood pressure was 120/70mmHg, and heart sounds were S1 and S2 only. The electrocardiogram showed complete heart block (shown in Figure 1).
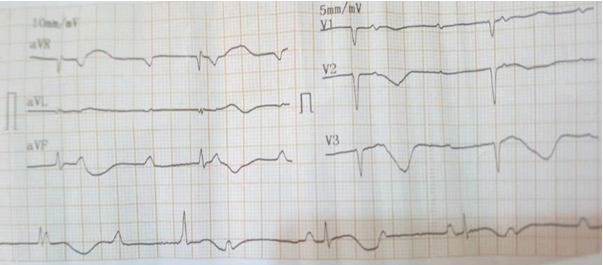
Figure 1. Complete Heart Block
His Na+=142mmol/l, K+=3.8mmol/l, urea=4.3mmo/l and creatinine=76µmmol/l. Informed consent was taken for dual chamber pacemaker implantation. This procedure was done on the 3rd of August, 2019. The pulse generator (Ensura DR MRI EN1DR01, Medtronic) was implanted in the left pectoral region with the right ventricular (RV) lead positioned in the right ventricle and the right atrial (RA) lead positioned in the right atrium close to the right atrial appendage (shown in Figure 2). Procedure was uneventful and patient was discharged home on the 6th of August, 2019.
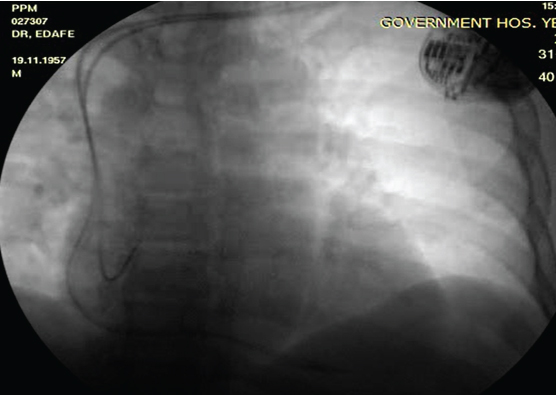
Figure 2. Final Fluoroscopy Image of the Implanted Dual Chamber Pacemaker on The 3rd Of August, 2019
Five weeks after the procedure, he developed sudden onset of hiccup and rhythmic contraction of the abdominal muscles. This continued for 12 hours without abating before he contacted the cardiovascular centre. He was asked to report to the hospital immediately. At presentation, he was hemodynamically stable and pulsations over the right upper abdominal area were visible. These contractions were observed while the patient was in standing and supine positions (video 1: showed abdominal contraction for every pacemaker beat).
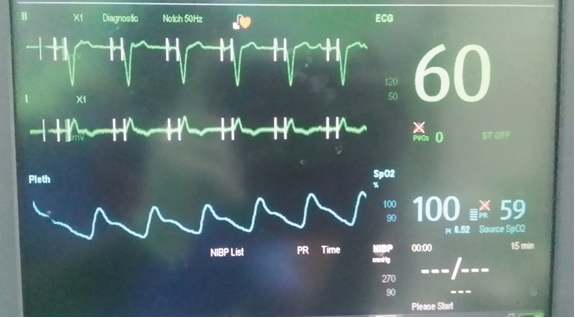
Interrogation of the device showed it was pacing both the right atrium and right ventricle; however, high atrial pacing thresholds were recorded in the pacemaker diagnostics and as a result it paced the right atrium at 5.00V @ 0.4ms. Atrial lead impedance was 342ohms. Also, there was loss of atrial sensing and intermittent loss of atrial capture seen on the continuous ECG of the patient and (ventricular) pulse rate was 60bpm (shown in Figure 3).
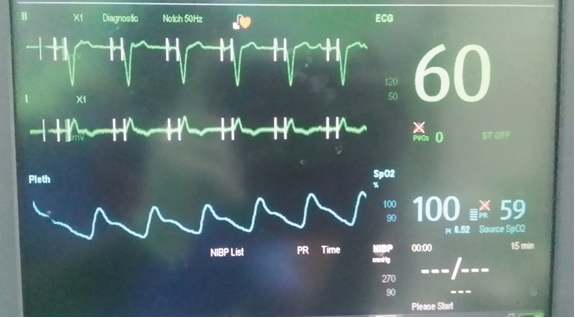
Figure 3. Loss of Atrial Sensing and Capturing
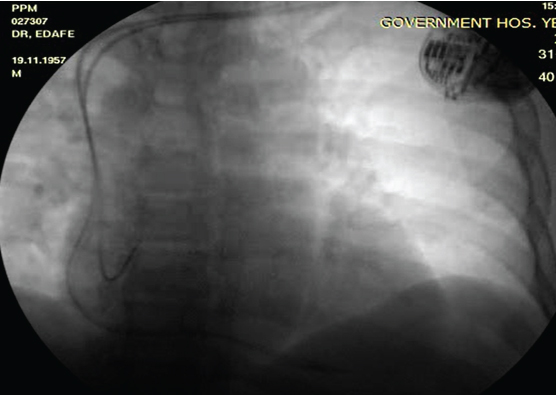
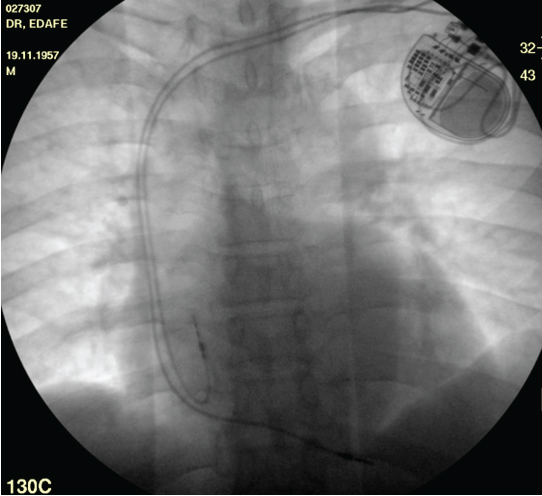
Under fluoroscopy, the atrial lead was found to have dislodged into the superior vena cava (shown in Figure 4). Prior to prepping the patient for atrial lead repositioning, the device was reprogrammed to VVI mode and the rhythmic contractions of the right hemi-diaphragm stopped immediately.
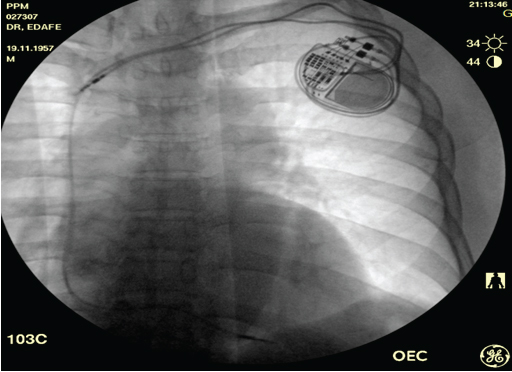
Figure 4. Displaced Right Atrial Lead At The Proximal Segment Of Superior Vena Cava. This Was Taken Before Start of Procedure
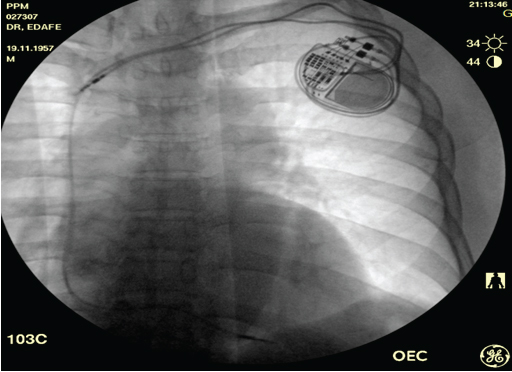
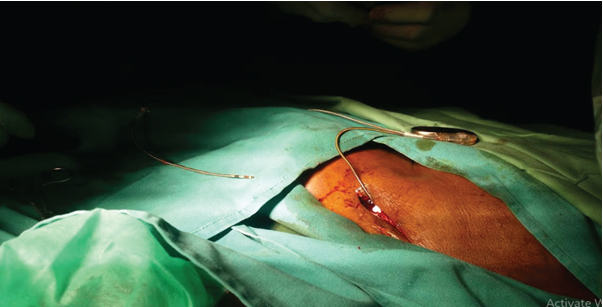
Procedure: Informed consent was taken after explaining to the procedure to the patient. Patient was prepped and the dislodged atrial lead was removed and replaced with a new atrial lead (CapSureFix Novus MRI SureScan 5076-52cm, Medtronic) which was positioned in the right atrium (shown in Figure 5 and 6).
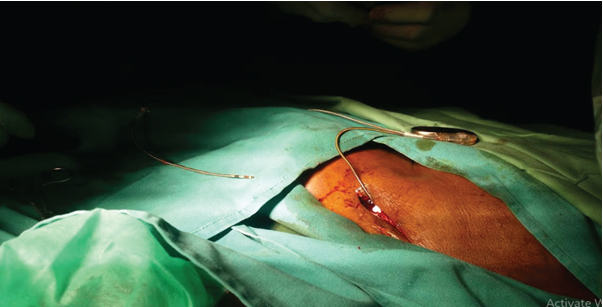
Figure 5. During the Removal and Repositioning of the Atrial Lead
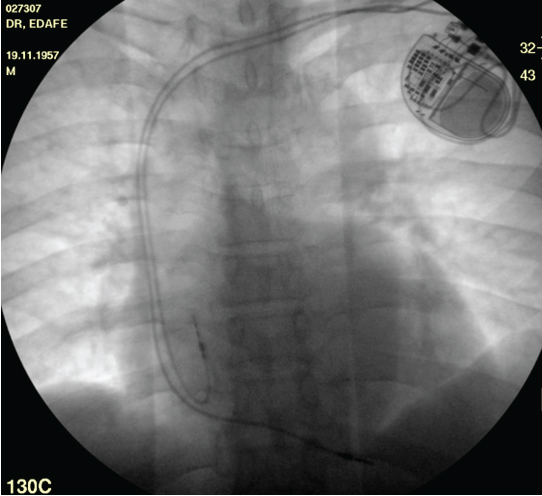
Figure 6. Final Fluoroscopy Image of the Implanted Dual Chamber Pacemaker after the Atrial Lead Was Replaced and Repositioned
Intra-operatively, measured P wave amplitude was 3.7mV at 0.4ms and atrial lead impedance was 380ohms. Diaphragmatic pacing test (10V) was done, and it was negative. The device was afterwards reprogrammed to DDD mode, and atrial output was reduced to 3.50V at 0.4ms (Implant data are shown in table 1 and 2). The patient was discharged two days after atrial lead repositioning.
Table 1 and 2 show the Implant data
Table 1: Final Implant Parameter Values Before the Pocket Was Closed
Parameters |
Atrial |
Ventricular |
Threshold |
0.4volts |
0.5volts |
R wave/ P wave |
16.2volts |
4.6volts |
Impedance |
320ῼ |
460ῼ |
Diaphragmatic pacing at 10 volts |
nil |
nil |
Lead stability and current of injury |
good |
good |
Table 2. Information of Device Implanted
Parameter |
Pulse generator |
Ventricular lead |
Atrial lead |
Manufacturer |
Medtronic |
Medtronic |
Medtronic |
Name |
Sphera DR MRI |
CapSure Fix Novus |
CapSure Fix Novus |
Model number |
SPDR01 |
5076-58 |
5076-52 |
Serial number |
FNC00422IG |
PJN9268868 |
PJN9287526 |
Phrenic nerve stimulation can be continuous or paroxysmal and can cause dyspnea, uncomfortable muscle twitching, hiccups and general malaise. Phrenic nerve stimulation could cause substantial discomfort to the patient [4, 5]. Pacemaker-induced extra cardiac stimulation causes involuntary muscle twitching, which involves the pectoral and intercostal muscles and the diaphragm [6-9]. Muscle twitching is one of the complications caused by a permanent cardiac pacemaker [6, 10]. Diaphragmatic stimulation may indicate direct stimulation of the diaphragm (left-sided) through a thin ventricular wall or less commonly, through a perforated ventricle. In the former case, reduction of output may relieve the problem [1]. Our patient had continued hiccup from the right phrenic nerve stimulation by the displaced atrial lead.
Pacemaker-induced twitching could also result from spontaneous migration of pacemaker leads or generator, cardiac perforation, inappropriate output and electric current leakage [11-13]. Hence the position, morphology and settings should be checked in a patient with unexpected muscle twitching with an implanted pacemaker [3]. In the present case, atrial, but not ventricular, pacing caused diaphragmatic stimulation by pacing the right phrenic nerve. This was observed on fluoroscopy when the patient presented to the cath lab. The atrial lead had been displaced to the SVC proximal segment. The diaphragmatic stimulation disappeared immediately the DDD mode was switched to VVI mode.
Complications have been reported in up to 9% of atrial lead placements. They are most often related to obtaining venous access (haemorrhage, pneumothorax: 2%) lead dislodgement (4.2%), inadequate pacing and sensing (3.5%) and acute pericarditis (5% in patients receiving active fixation atrial leads) [1].
In the present case, the dislodged atrial lead caused the rhythmic contractions of the right hemi-diaphragm. The pacemaker was pacing the right atrium at 5.00V @ 0.4ms due to high atrial pacing threshold, atrial lead impedance was 342ohms, pulse rate was 60bpm and there was loss of atrial sensing and intermittent loss of atrial capture seen on the patient's continuous ECG (Figure 3). This indicated atrial lead dislodgement. This was confirmed under fluoroscopy which showed that the atrial lead tip has dislodged into the superior vena cava (just below the union of the right and left brachiocephalic veins to form the SVC). As reported by Khan et al. [9] because the immediate medical relations of the right phrenic nerve in the chest are the right brachiocephalic vein, the superior vena cava, the right atrium, and the inferior vena cava; stimulation of the right phrenic nerve would have been the cause of diaphragmatic twitching. Stimulation of the right phrenic nerve by an atrial pacing electrode displaced into the SVC in a pacemaker Twiddler has been recognized [9]. Reprogramming the device mode to VVI immediately stopped the diaphragmatic twitching. The dislodged atrial lead was removed and replaced with a new atrial lead. Testing of diaphragmatic pacing at 10V was done and no rhythmic contractions of the diaphragm were observed. The device mode was afterward reprogrammed to DDD.
We describe a patient with a permanent pacemaker implanted for complete heart block who presented with sudden onset of right diaphragmatic contraction. Atrial lead was displaced to the superior vena cava where it was pacing the right phrenic nerve. The device was programmed to VVI mode to abolish the hiccup. A new atrial lead was repositioned and the device mode was changed to DDD afterwards.
We deeply appreciate the assistance of Bayelsa Specialist Hospital management
The authors will fund this article from their personal fund. We have no support from any one in funding the article.
None
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
- Namazi MH, Karbasi Afshar R, Safi M, et al (2008) Diaphragmatic Stimulation: A case of Atrial Lead Dislodgement and Right Atrium Perforation. Indian Pacing Electrophysiol J 8: 133-136. [Crossref]
- Grier D, Cook PG, Hartnell GG (1990) Chest radiographs after permanent pacing. Are they really necessary? Clinical radiology 42: 244-249. [Crossref]
- Ostrowska M, de Carvalho M (2015) Injuries of the Nerves of the Thorax. In: Nerves and Nerve Injuries 525-543. [Crossref]
- Moubarak G, Bouzeman A, Ollitrault J (2014) Phrenic nerve stimulation in cardiac resynchronization therapy. J Interv Card Electrophysiol 41: 15-21. [Crossref]
- Shah R, Qualls Z (2016) Diaphragmatic stimulation caused by cardiac resynchronization treatment. CMAJ 188: E239-E239. [Crossref]
- Tanabe K, Kotoda M, Nakashige D (2019) Sudden onset pacemaker-induced diaphragmatic twitching during general anesthesia. JA Clinical Reports 5: 36. [Crossref]
- Bozyel S, Aksu T, ErdemGuler T, et al. (2017) Pectoral muscular twitching: a rare manifestation of spontaneous Twiddler syndrome. J Geriatr Cardiol 14: 532-533. [Crossref]
- Erdogan O (2007) Intercostal muscle twitching: an unusual manifestation of extra cardiac stimulation related to right ventricular outflow tract pacing. Can J Cardiol 23: 815-816. [Crossref]
- Khan AA, Nash A, Ring NJ, et al. (1997) Right hemidiaphragmatic twitching: a complication of bipolar atrial pacing. Pacing Clin Electrophysiol 20:1732-1733. [Crossref]
- Bayliss CE, Beanlands DS, Baird RJ (1968) The pacemaker-Twiddler’s syndrome: a new complication of implantable transvenous pacemakers. Can Med Assoc J 99: 371-373. [Crossref]
- Catherwood E, Elzawahry MK, Kotler MN, et al. (1979) Dislodgment of pacemaker electrode simulating focal motor seizure. Chest 75: 627-628. [Crossref]
- Ahmed A, Shokr M, Lieberman R (20177) Sub acute right ventricular perforation by pacemaker lead causing left-sided hemothorax and epicardial hematoma. Case Rep Cardiol 2017:1264734 [Crossref]
- Suri A, Malik A, Reinthaler M, et al. (2013) Abdominal skeletal muscle twitching due to current leak from a pacemaker extension connector box. Heart Asia 5: 259. [Crossref]