Spondylotic myelopathy, also known as Cervical myelopathy disorder, is characterized by spinal cord dysfunction due to compressed forces.
It is considered a common spinal disorder but is still underdiagnosed or late diagnosed. Its epidemiological data on incidence and prevalence is limited, affecting up to 5% of the population older than 40 years, driving high morbidity in care settings.
This context led us to present a case of a 37-year-old female patient living with cervical myelopathy.
Spondylotic Myelopathy; Cervical Myelopathy; Spine Pathologies; Surgical Approach; Case Report
Worldwide the prevalence of cervical spine pathologies is increasing along with the aging population; it is associated with substantial morbidity [3]. Evidence indicates that up to 5% of the population over forty years is affected by Cervical myelopathy [1].
This disease, also known as cervical spondylotic myelopathy disorder, is a dysfunction characterized by compressed forces on the spinal cord. It is considered a common spinal disorder but still underdiagnosed or late diagnosed and evidence of its incidence and prevalence is limited [2]. Brazil is not the exception, and epidemiological data is also scarce [4].
Considering this context, we present a clinical case that caught our attention in a 37-year-old female patient with cervical myelopathy diagnostic.
Patient Information and Findings of Physical Examination
In January 2022, a 37-year-old female housewife was admitted to our hospital for the first time with a 2-year history of neck pain, and six months ago, she began to experience pain in the neck region that radiated to both limbs. Upper limbs, paresthesia in the forearm and hand of non-specific dermatomal distribution, difficulty handling thin objects, and changes in gait.
The patient had received therapy of traditional pharmacological drugs to alleviate the pain, with coadjuvant physiotherapy.
The examination showed cervical and dorsal paravertebral muscles had pain and stiffness trigger points, also bilateral hypoesthesia with a distribution of C4-C5 and C5-C6 roots. Using the Medical Research Council (MRC) Scale for Muscle Strength, the degree of muscle strength showed a force power of 4/5 for elbow flexion and bilateral wrist extension for the lower limbs 5/5.
Tonus was spastic in both the upper and lower limbs, maintaining deep tendon reflexes. The patient had a broad base gait with a negative Romberg sign. Positive Hoffmann sign and Babinski reflex on both sides.
The Modified Japanese Orthopedic Association scale (mJOA) score was 13, suggesting moderate myelopathy.
Diagnostic Assessment
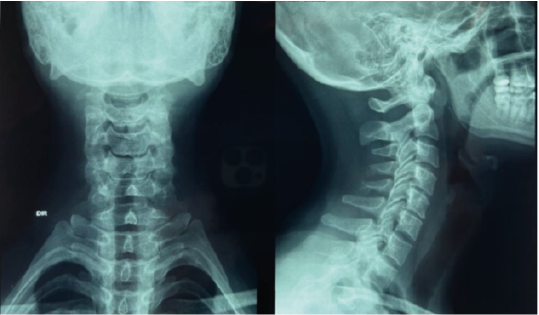
The radiographic of the Cervical spine (Figure 1) and cervical spine extension and flexion (Figure 2) show: Anterior-posterior (AP) cervical spine radiography with preserved frontal alignment.
Profile: decreased C4-C5 and C5-C6 space with loss of disc height in these segments, small osteophytes in the anterior and posterior regions of the vertebral body at C4, C5, and C6, and decreased cervical lordosis.
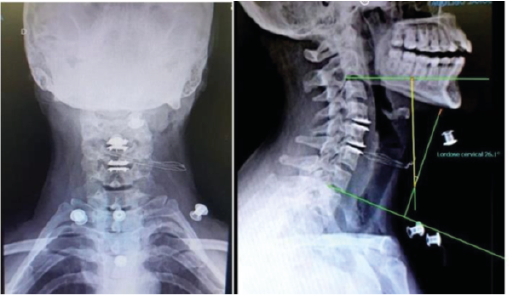
The dynamic X-rays evidence a flexible cervicalspine (figure 2) with no evidence of instability on lateral flexion-extension radiographs.
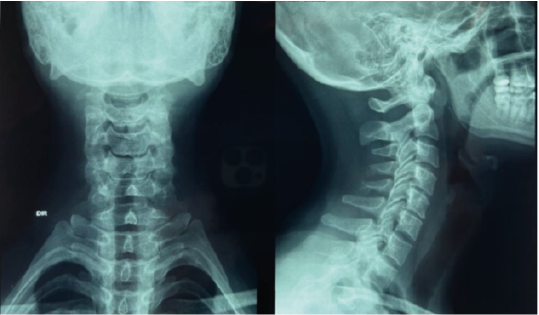
Figure 1: Cervical spine radiography

Figure 2: Dynamic cervical spine radiography
Magnetic resonance imaging of the cervical spine in the axial view at the level of C4-C5 (figure 3), axial view at the level C5-C6 (figure 4), and sagittal view (figure 5) evidence the cervical spine T2-weighted with vertebral bodies. Preserved height showing inversion of cervical lordosis with disc protrusion at C4-C5 and C5-C6.
Levels of C4-C5 and C5-C6 with Pfirrmann IV with a sign of myelopathy at these levels, a sign of dehydration of the cervical intervertebral discs (Pfirrmann II) in levels C2-C3 and C3-C4, facets and uncovertebral joints of normal appearance.
C4-C5 with central disc protrusion compressing and deforming the anterior surface of the dural sac and the spinal cord, not visualizing the anterior cerebrospinal fluid column at this level, with bilateral foraminal sub-stenosis.
C5-C6 showed central disc protrusion compressing and deforming the anterior surface of the dural sac, not visualizing the anterior cerebrospinal fluid column at this level, with foraminal sub-stenosis on the right. The paravertebral structures present a normal appearance.

Figure 3: Magnetic resonance imaging of the cervical spine level C4-C5

Figure 4: Magnetic resonance imaging of the cervical spine level C5-C6

Figure 5: Cervical spine magnetic resonance sagittal section
Therapeutic Management
As conservative measures of pharmacological and non-pharmacological treatment could not alleviate the patient's symptoms, surgical treatment was the only option. An anterior cervical approach was performed with discectomy at levels C4-C5 and C5-C6 with the replacement of the intervertebral discs with disc prostheses (M6-C, Spinal Kinetics).
It was preferred to place the prosthesis in the most anterior portion of the intradiscal space for better correction of the cervical lordosis angle (Figures 6 and 7). After the surgery, the patient presented no complications and was discharged from the hospital in two days.

Figure 6: Intraoperative radioscopy of the cervical spine after disc prosthesis
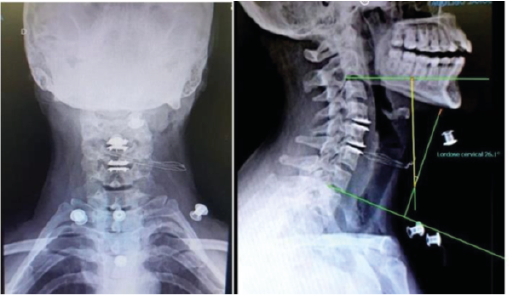
Figure 7: X-ray s of the cervical spine in outpatient follow-up
Post-Operative and Patient Follow-Up
In the 3-month outpatient follow-up, a significant improvement in the symptoms of neck pain, paresthesia, hand function, and gait was observed. The mJOA score in this outpatient follow-up was 16.
Most cases of Cervical spondylosis are asymptomatic. In symptomatic patients, the diagnosis is based on neck pain, and its clinical location is difficult even in severe cases because of the ample overlapping of nerve supplies in dermatomes.
The symptoms can develop acutely when herniation of the nucleus pulposus of the intervertebral disc, causing paresthesias or tingling in the nerve root distribution in 80% of patients [5].
In Brazil, the Ministry of Health approved the Clinical Protocol and Therapeutic Guidelines to treat Spondylosis [4]. In addition, based on patient evolution, various non-pharmacological strategies exist to manage pain [8]. However, when the non-surgical measures are insufficient to improve the patient's condition, surgical spinal cord decompression is recommended for patients with symptomatically moderate to severe stages or with neurological deficits [6]. The primary surgery goal is to decompress the spinal cord. Abnormalities of the cervical curvature can destroy the spine with negative consequences on biomechanical function, including muscle damage, bone hyperplasia, and cervical spondylosis [7, 9]. Arthrodesis used to be the gold standard of treatment for degenerative disc disease, but this concept has been changing, and arthroplasty for cervical degenerative disc disease for 1 or 2 levels is increasing its use.
The clinical results of arthroplasty and arthrodesis are similar in the first five years, with the advantage of arthroplasty maintaining mobility in the operating segment. The significant advantage of cervical arthroplasty is that it does not overload the segments adjacent to the procedure, reducing symptomatic degenerative disease of the adjacent segment and the rate of reoperation in the medium and long term. The remarkable ability of third-generation arthroplasty to create cervical lordosis, rebalancing cervical alignment in the sagittal plane.
Due to the reasons mentioned above, the surgeon's team decided to treat the patient with a 2-level arthroplasty. This surgical approach improved the patient's cervical lordosis, from 19° to 26°, measured by Cobb angle, resulting in neck pain relief and improvement of her quality of life.
It is essential to individualize the therapeutic plan for each patient suffering from cervical myelopathy. A timely and appropriate diagnosis is crucial to preventing clinical relapse.
Surgical intervention is recommended to treat moderate to severe cases, decompress the spinal cord, and maintain spine alignment and its mechanical stability in the long term.
- The Lancet Neurology (2019) A Focus on patient outcomes with cervical myelopathy. Lancet Neurol 18: 615. [Crossref]
- Andrew S. Zhang., Christopher Myers., Christopher L. McDonald., Daniel Alsoof., George Anderson., et al. (2022) Cervical Myelopathy: Diagnosis, Contemporary Treatment, and Outcomes. Am J Med 135: 435- 443. [Crossref]
- Waheed MA., Hasan S., Tan LA., Bosco A., Reinas R., et al. (2020) Cervical spine pathology and treatment: a global overview. J Spine Surg 6: 340-350. [Crossref]
- Ministry of Health (2013). Clinical Protocol and Therapeutic Guidelines of Spondylosis.
- Robinson J., DO K (2009) Clinical features and diagnoses of cervical radiculopathy.
- Fehlings M., Tetreault L., Aarabi B (2017) A clinical practice guideline for the management of patients with acute spinal cord injury: Recommendations on the type and timing of rehabilitation. Global Spine J 7: 231S-238S. [Crossref]
- Boerger TF., Hyngstrom AS., Furlan JC., Kalsi-Ryan S., Curt A., et al. (2022) Developing Peri-Operative Rehabilitation in Degenerative Cervical Myelopathy [AO Spine RECODE-DCM Research Priority Number 6]: An Unexplored Opportunity? Global Spine J 12: 97S-108S. [Crossref]
- Harvey L., Glinsky J., Bowden J (2016) The effectiveness of 22 commonly administered physiotherapy interventions for people with spinal cord injury: A systematic review. Spinal Cord 54: 914-923. [Crossref]
- Hsu W., Dorsi MJ., Witham TF (2009) Surgical Management of Cervical Spondylotic Myelopathy. Neurosurg Q 19: 302-307. [Crossref]