Introduction: A case control study with a sample size 117 of patients with COVID-19 infection was investigated in order to examine the benefit of usage of anticoagulants in a retrospective manner in the state of Florida. Recently, researchers found that COVID-19 is associated with a higher incidence of thrombosis than the general population. There are various mechanisms proposed for thrombosis development, most of which are still not fully understood. The addition of anticoagulants during treatment for COVID revealed a significant mortality benefit, about 8% died in the case group including 80% of who did not receive anticoagulant. In contrast, 37% died in the control group, 4 (80%) out of 5 patients whom survived were already on anticoagulants prior to the admission. A significant P value has been seen with 0.0001, OR 41.2 and CI 95%.
Background and objective: The aim of the study is to assess the fundamental roles of anticoagulants in treatment of COVID-19 patients and an improvement of the survival rate. The goal is to provide a statistical evidence that anticoagulants correlate with an improvement of the survival rate and reduce the hospitalization.
Method: Case-Control Study was conducted in COVID-19 patients and admitted to hospital. The data was obtained from two different hospitals in Florida for the year 2020-2021. Total of 117 patients were included in the study and where assigned to either the case group or the control group. In the case group; there were 65 patients versus 52 patients in the control group.
Results: In one hundred seventeen patients, 53 out of 65 patients in the case group received anticoagulants, while only 5 out of 52 in control group were already on anticoagulants secondary to medical conditions. Additionally, 24 patients died, however only 5 out of 65 patients in case group versus 19 out of 52 in control group, such implementation suggests a decrease in mortality rate with the use of anticoagulants.
Conclusion: The usage of anticoagulants in COVID-19 patients provided a drastic decline in mortality rate and reduced patient’s hospitalization.
As far as the COVID-19 cases surging every month during this pandemic and still no proven treatment have been found yet, the role of anticoagulants can help to reduce the mortality based on the causes that have been found in the autopsy of the deceased patients. The major complications of COVID have been including thrombosis, acute respiratory distress syndrome, as well as other complication. COVID-19 is a respiratory disease caused by SARS-COV-2 that originated in China in 2019 led to a pandemic in a short period to infect various age groups with a high mortality rate. The virus is transmitted via respiratory droplets among patients. There are various clinical presentations that range from mild to severe and even death [1].
The clinical presentation of COVID-19 ranges from asymptomatic to severe life threatening acute respiratory distress syndrome (ARDS). COVID-19 affects multiple organ systems and disturbs the normal physiological process of the body. The novel virus continues to evolve, and researchers have concluded a significant correlation between the virus and coagulopathy via certain mechanisms including stimulation of coagulation cascade via direct versus indirect method [1, 2].
A retrospective case control study by reviewed the patients charts of patients whom been admitted to the hospital for COVID-19 infection between period of January 2020 to January 2021. A sample of 117 patients was included in the study. The study designed into two groups; the case group that included 65 patients whom infected with COVID versus the control group that included 52 patients whom infected with COVID as well.
The odd ratio was used to assess the association between anticoagulants and the mortality benefits. According to the study, the odd ratio was 41.51 with a 95% confidence interval (13.62-126.57, P value 0.0001) which means there is a significant evidence between the use of anticoagulants and mortality benefits as the p value was less than 0.05. However, if the OR = 1, means no association between them, OR > 1, means there is a strong association between them while if the OR <1, that means there is low association between them [3].
The study conducted 65 patients in the case group and 52 patients in the control group (see table 1).
Table 1: Comparison of Between Case Group versus Control Group Along With the P Value, Odd Ratio and the Confidence Interval
Variables |
Category |
Case |
Control |
P value |
OR |
95% CI |
Anticoagulation |
Yes |
53 |
5 |
0.0001 |
41.2 |
13.6 - 126.6 |
|
No |
12 |
47 |
|
|
|
Death |
Yes |
5 |
19 |
0.0004 |
0.15 |
0.05 - 0.043 |
|
No |
60 |
33 |
|
|
|
Hospitalization <7 Days |
Yes |
51 |
5 |
0.0001 |
34.3 |
11.45 - 102.4 |
|
No |
14 |
47 |
|
|
|
Male |
|
42 |
28 |
|
|
|
Female |
|
23 |
24 |
|
|
|
HTN |
Yes |
30 |
29 |
0.3 |
0.7 |
0.32 - 1.42 |
|
No |
35 |
23 |
|
|
|
DM |
Yes |
10 |
5 |
0.35 |
1.7 |
0.55 - 5.35 |
|
No |
55 |
47 |
|
|
|
Smoking |
Yes |
14 |
9 |
0.5 |
1.3 |
0.5 - 3.32 |
|
No |
51 |
43 |
|
|
|
Alcohol |
Yes |
55 |
35 |
0.03 |
2.7 |
1.09 - 6.5 |
|
No |
10 |
17 |
|
|
|
OR: Odd ratio
CI: Confidence Interval
DM: Diabetes Mellitus
HTN: Hypertension
The case group consisted of 65 patients including 42 males and 23 females, only 53 patients have received anticoagulants versus 12 patients did not receive it. In contrast, the control group consisted of 52 patients including 28 males and 24 females, only 5 patients have received anticoagulants versus 47 patients did not receive anticoagulants. Certain variables as we see above have not showing any statistical significances as the P values were larger than 0.05, for which a needing for further research and study are potentially going to happen in the near future. While, the P values for the rest of the variables were statistically significances, less than 0.05.
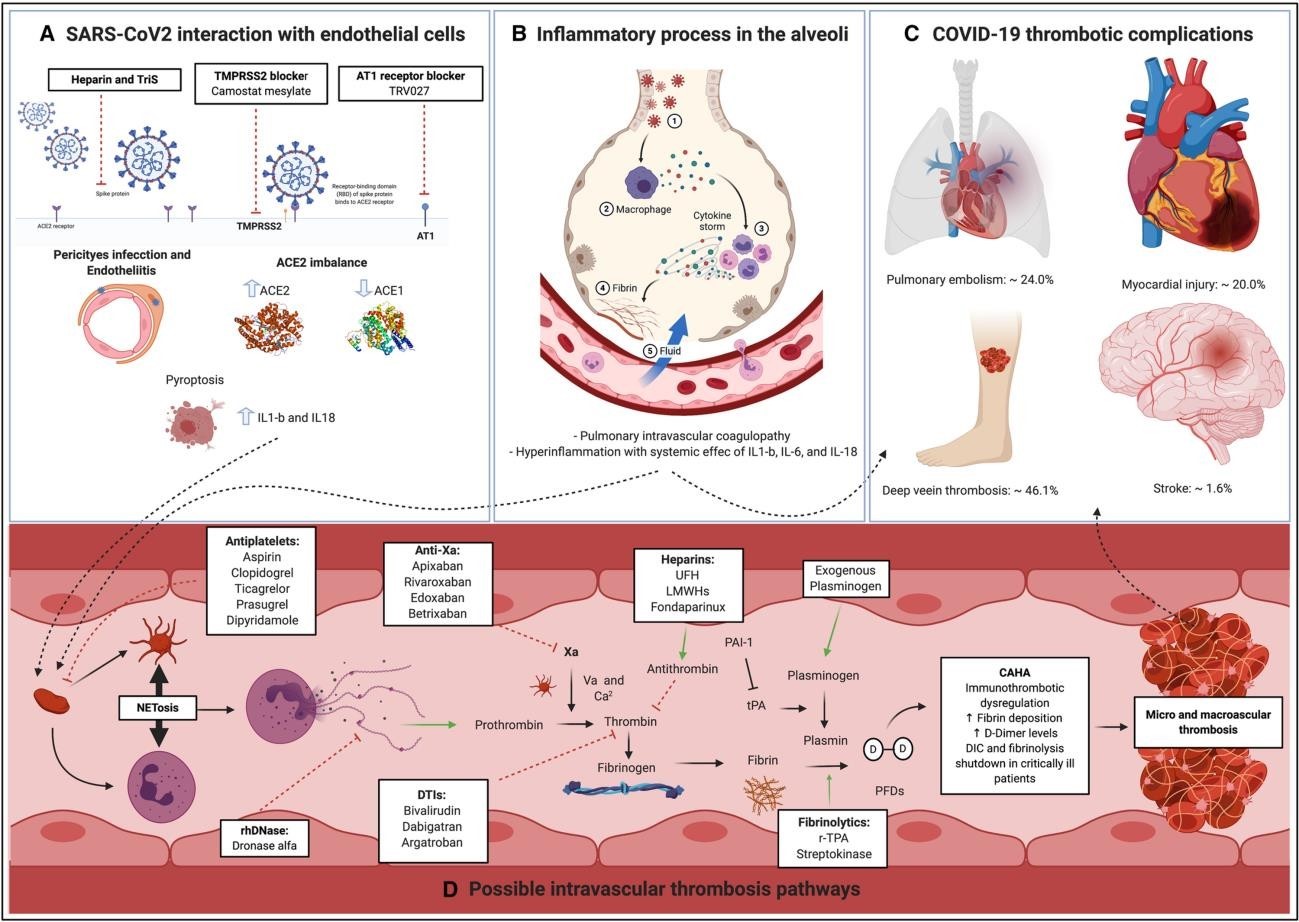
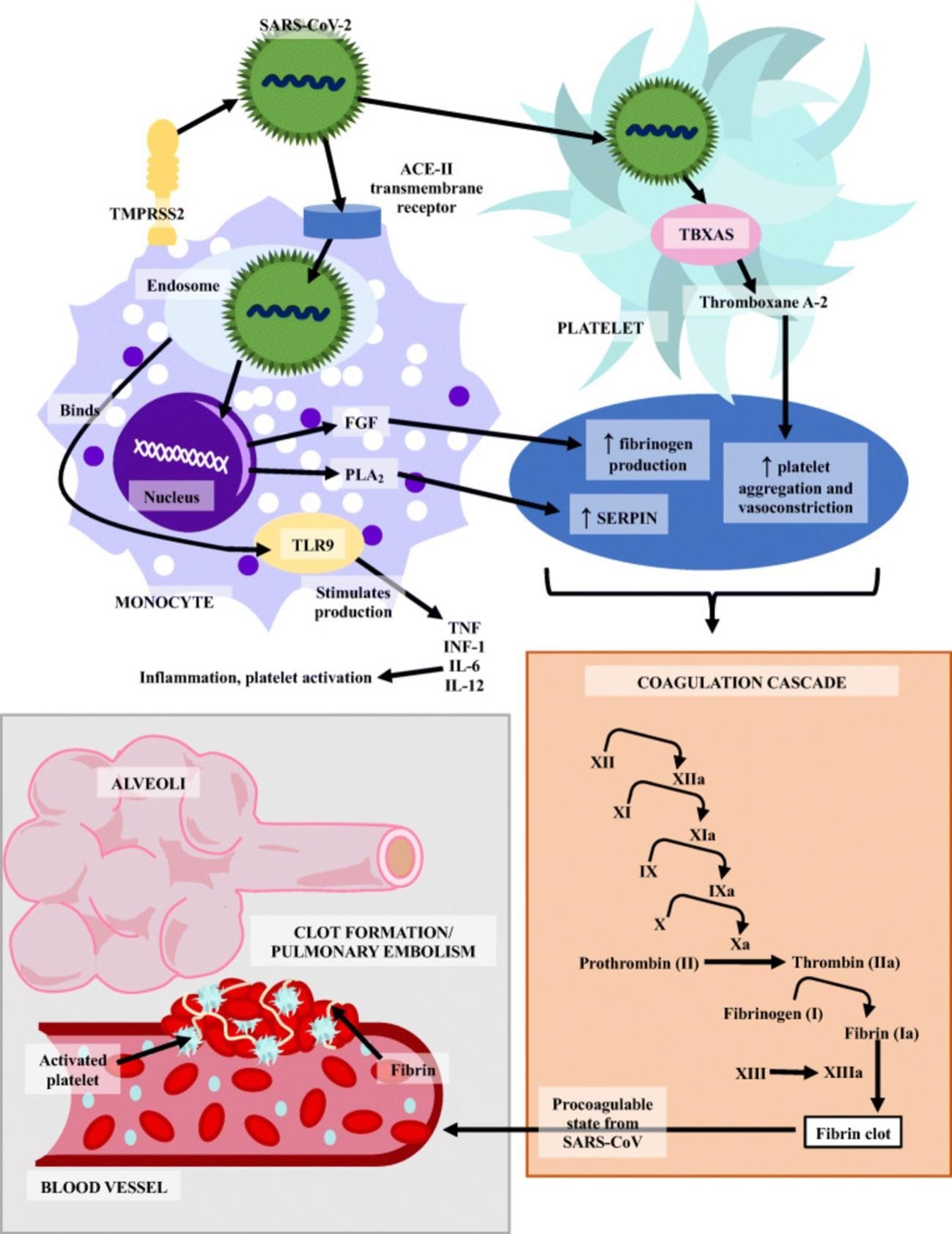
COVID-19 infection has had and continues to have a drastic negative impact on the entire population since 2019, with different ambiguous clinical scenarios. Every day, we know that different clinical picture comes as a consequence of COVID-19, but in this case, we will focus only on the hypercoagulable state associated with COVID-19. The pathophysiology behind the hypercoagulability is still mysterious and under investigation. There are several proposed mechanisms have been described recently involving disseminated intravascular coagulation. Suggested mechanism for hypercoagulable state includes anti-phospholipid syndrome, activation of complement cascade, Imbalance of ACE2 regulation, characteristic of the virus itself and endothelial dysfunction that is accompany by the virus [3]. The overall mortality and the prognosis have been studied in China and indicate that a patient who had a higher level of D-dimer, fibrin degradation product level, prolonged prothrombin time and partial thromboplastin time would be having a very poor prognosis compare to those without these changes [4]. Additionally, the New England Journal of Medicine recently published certain cases that tested positive for particular antibodies such as anti-IgA, anti-IgG, anti-cardiolipin, as well as anti-B2 glycoprotein IgA, which concluded that anti-phospholipid syndrome could be possible etiology [4]. Another study noted that COVID-19 associated with activation of complement cascade that led into diffuse thrombotic microangiopathy [4, 5]. Unfortunately, there is only a limited understanding behind the concept of hypercoagulability that is associated with COVID-19 (See Figure 1 and 2).
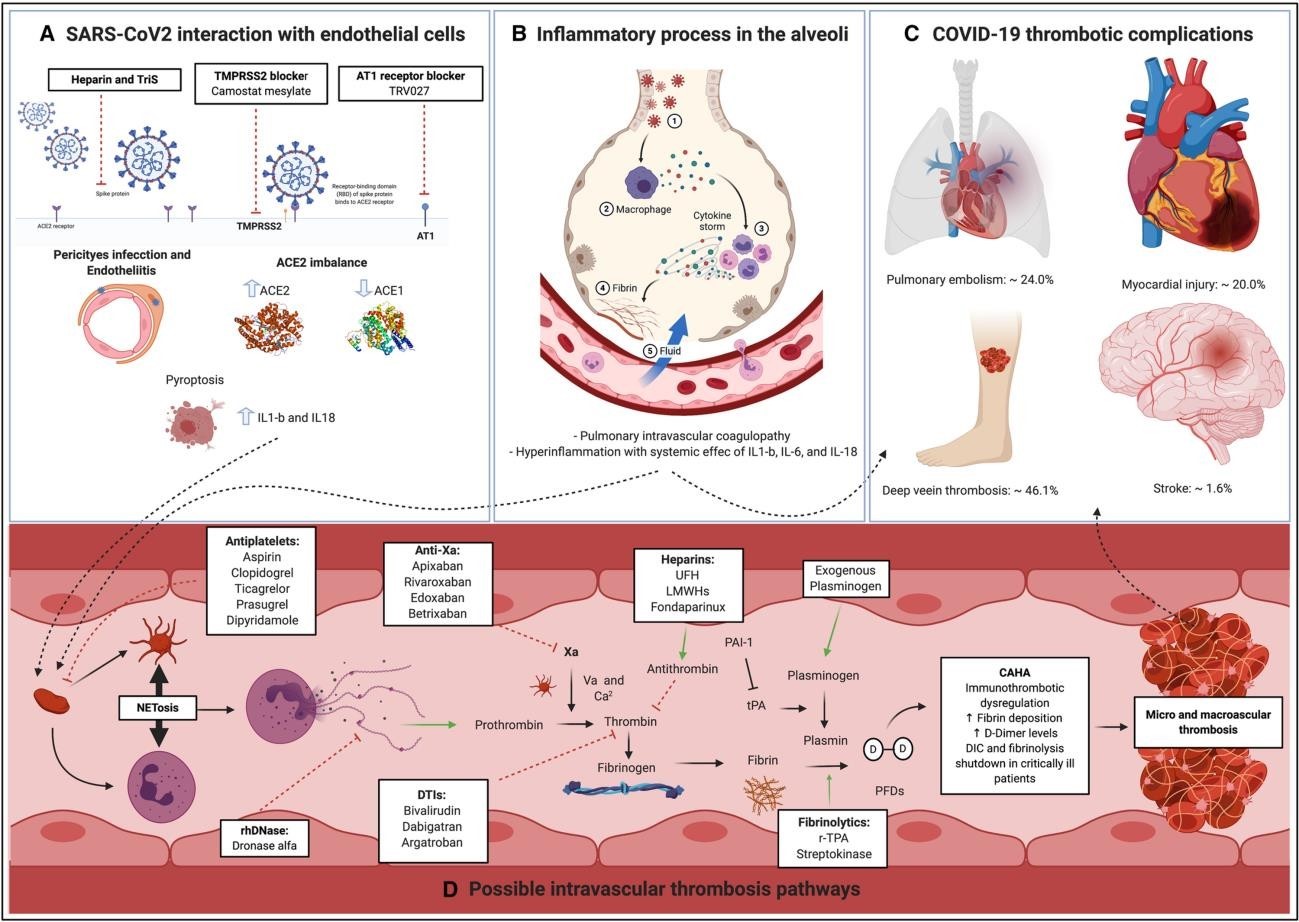
Figure 1: Pathophysiological Mechanism of Hypercoagulability in COVID-19
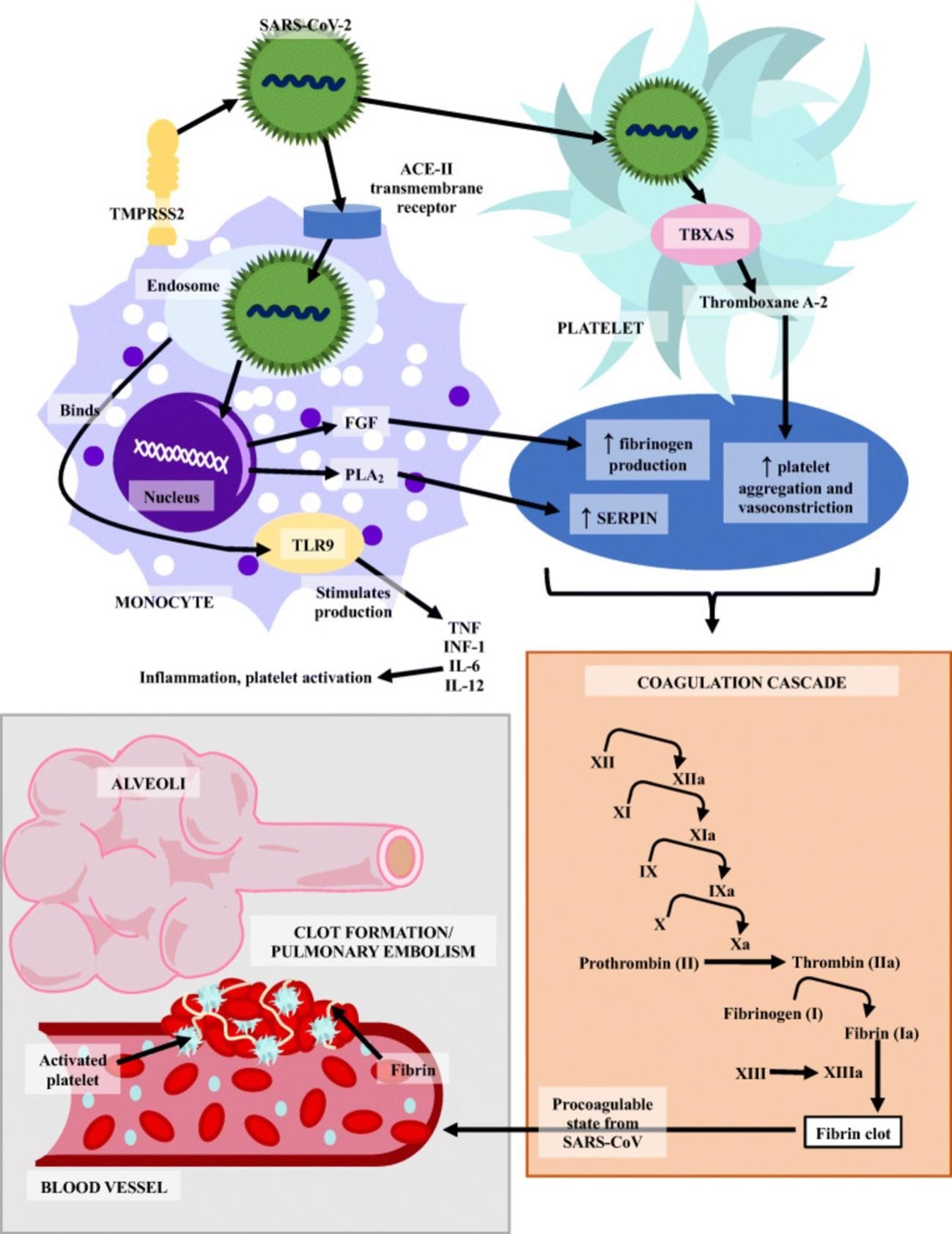
Figure 2: The Cartoon above Explaining the Steps of Hypercoagulability in Coronavirus Infection
Corona virus uses the spike protein (S) to bind to TMPRSS2 receptor, which allows the virus to enter the cell via ACE-2 receptor [6]. This mechanism occurred also in SARS-CoV-1, and there is in vitro study that revealed certain genes have been overexpressed including Serin Protease, Fibroblast Growth Factor (FGF) along with Fibrinogen Gamma Chain that could potentially lead to activation of coagulation agents including factor two, three, and ten, and ultimately ended up with thrombophilia [7].
The mortality of COVID-19 has been correlated with pulmonary and peripheral hypercoagulability for the mechanism that mentioned earlier. Interestingly, the dysregulation of the inflammatory reaction via cytokine storm or macrophage activation syndrome led to pulmonary microthrombi that have been noticed by an autopsy [8]. Certain hypothesis claims that plasmin can potentially participating in furin places cleavage of the spike that located on the surface of COVID-19 virus, thus the D dimer levels have been elevated [9]. However, a cohort study of 184 patients in the ICU in Netherlands revealed an incidence of 31% of thromboembolic events among those patients. Given that said, they were highly recommended to utilize certain anticoagulants in all patients whom attracted COVID-19 infection [10].
Our research has been focused on the incidence of COVID-19 associated with thrombophilia. The patients whom received anticoagulant have been shown a significant mortality benefit and decrease the duration in the hospital compared with patients whom had have not received anticoagulants with a significant P value of 0.0001 in a retrospective case-control study.
- Rico-Mesa JS., Rosas D., Ahmadian-Tehrani A., White A., Anderson AS., et al. (2020) The Role of Anticoagulation in COVID-19-Induced Hypercoagulability. Springer 22:53. [Crossref]
- Szumilas M (2010) Explaining odds ratios. Journal of Canadian Academy of Child and Adolescent Psychiatry 19: 3. [Crossref]
- Ning Tang., Dengju Li., Xiong Wang., Ziyong Sun (2020) Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. Journal of thrombosis and hemostasis 18: 4. [Crossref]
- Yan Zhang., Meng Xiao., Shulan Zhang., Shuyang Zhang., Yongzhe Li (2020) Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19. The New England Journal of Medicine 382: 38. [Crossref]
- Courtney M Campbell., Rami Kahwash (2020) Will Complement Inhibition Be the New Target in Treating COVID-19-Related Systemic Thrombosis?. The New England Journal of Medicine 141:22. [Crossref]
- Markus Hoffmann., Hannah Kleine-Weber., Simon Schroeder., Nadine Krüger (2020) SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 181:16. [Crossref]
- Dimitrios Giannis., Ioannis A Ziogas., Panagiota Gianni (2020) Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. Journal of Clinical Virology 127: 7. [Crossref]
- Juan Simon Rico-Mesa., Averi White., Allen S Anderson (2020) Outcomes in Patients with COVID-19 Infection Taking ACEI/ARB. Springer 14: 5. [Crossref]
- Hong-Long Ji., Runzhen Zhao., Sadis Matalon., Michael A Matthay (2020) Elevated Plasmin(ogen) as a Common Risk Factor for COVID-19 Susceptibility. American Physiological Society 100: 3. [Crossref]
- F A Klok., M J H A Kruip., N J M van der Meer., M S Arbous., D A M P J Gommers (2020) Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thrombosis Research 191: 18. [Crossref]