First permanent molars are most likely to be affected by dental diseases because of early exposure to the oral environment and poor condition and an unfavorable long-term prognosis may require its extraction in later life. In such cases, past report suggested the autogenous tooth transplantation using impacted wisdom tooth is effective. But there are few reports mentioned about long-term prognosis after the treatment. This time we experienced the 5 cases of autogenous wisdom tooth transplantation in young patients with pulp vital signs shown after treatment with 3 to 7 years of follow-up. These long-term prognosis of our 5 cases showed that auto transplantation using an impacted third molar is suggested to be an alternative method for treatment of a lost molar in a young patient.
Autogenous wisdom tooth transplantation; Tooth migration; Pulp vital sign
Tooth auto-transplantation is a technique used to reposition an autogenously, partially, or unerupted tooth from one side to the other. It is a valuable treatment option for replacing a missing tooth or one that requires extraction due to dental caries, periodontal disease, or other condition [1,2].
First permanent molars are most likely to be affected by dental caries because of early exposure to the oral environment. Due to the relatively high level of organic contents in a newly erupted tooth, its immature enamel is more permeable and therefore more susceptible to caries [3]. Consequently, more than 50% of children over 11 years old have dental caries in these teeth. Heavy restoration of an affected tooth because of poor condition and an unfavorable long-term prognosis may require its extraction in later life [4], thus leading to unfavorable occlusal changes if the resultant space is left unrestored. However, it is not possible to use a definitively shaped prosthesis, such as dental implant or fixed bridge prosthesis, in young patients during the growth period even if they have lost a permanent molar tooth. In such cases, a removable partial denture is sometimes used as a space retainer. On the other hand, most such young patients possess wisdom tooth germs, which are generally available for auto-transplantation for missing tooth replacement. Andreasen et al. reported that the vital signs of a donor tooth can be seen after wisdom tooth auto-transplantation in young patients [5], thus eliminating the need for root canal treatment. In addition, Waldon et al. found a high success rate for auto-transplantation as well as its value as an ideal natural space maintainer for preserving alveolar bone, gingival tissue, and space in the dental arch.
A good result following auto-transplantation is dependent on careful case selection and an understanding of the biological factors related to attainment of an apical seal, which is essential for normal function. High rates of success have been reported in cases in which the donor third molar has been transplanted prior to complete root formation [6]. Furthermore, successful auto-transplantation of teeth with complete root development has been commonly reported. Nevertheless, unresolved issues related to auto-transplantation remain, such as long-term prognosis, changes in dental pulp tissue, and tooth migration as a result of growth in young patients.
Here, we present findings related to long-term prognosis of the donor tooth in cases of tooth auto-transplantation, in which surgical skill, as well as specific knowledge and acquired information for successful transplantation obtained in clinical practice were applied.
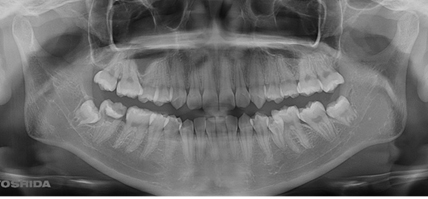
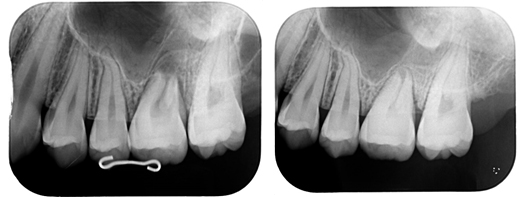
A representative case is presented, including details regarding our surgical technique. A 17-year-old female had spontaneous pain in the mandibular right second molar (FDI notation #47) and was referred to Tanpopo Dental Clinic in 2013. An extra-oral examination showed no facial swelling or palpable lymph nodes. Intra-oral examination findings revealed no sinus tract and no periodontal pocket, while the clinical crown of tooth #47 was severely destroyed to the under subgingival level. The prognosis of the affected tooth was considered to be hopeless due to severe damage to the coronal tooth structure (Figure 1). Radiographic imaging revealed unsatisfactory previous endodontic treatment, along with a periapical lesion and broken lamina dura. The diagnosis was a combined periodontal and endodontic lesion. Panoramic X-ray results showed a premature mandibular right third molar with half of the root in a development stage, according to Moorrees’ classification, and completely impacted, thus it was considered to be a proper candidate for auto-transplantation (Figure 2).

Figure 1. Occlusal view, first medical examination. The right second molar (#47) showed severe decay.
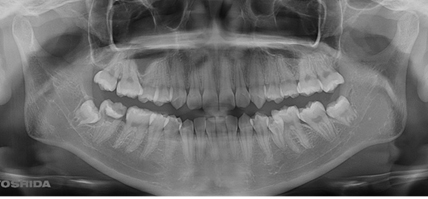
Figure 2. Panoramic X-ray findings. The immature tooth germ of #48 was shown next to #47.
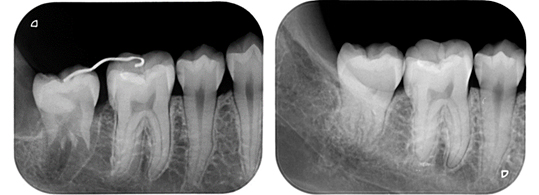
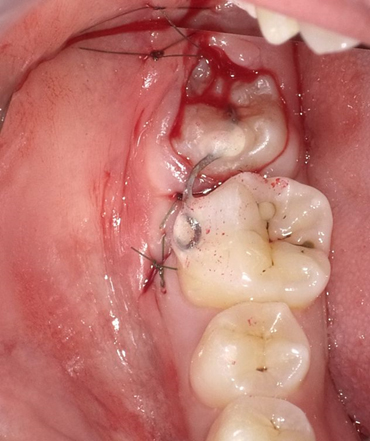
A complete explanation of the procedure, as well as its risks and benefits were presented to the patient and necessary permission was obtained. A 0.05% chlorhexidine gluconate solution was used for oral disinfection. Oral surgery was performed under local anesthesia, with an inferior alveolar nerve block used for tooth #47 with 2% lidocaine and 1:80000 epinephrine (Dentsply, Japan). The mandibular right second molar was extracted in an atraumatic manner without any bone removal. Extraction was performed with a straight elevator and the socket was prepared by sterile saline irrigation. A triangular flap design provided excellent access to the surgical site. Tooth #48 was extracted without trauma and a minimum amount of distal bone removed. The extracted donor tooth was kept in sterile wet gauze for less than 15 minutes, then placed into the recipient socket. After transplanting the donor tooth, it was splinted with rectangular wire and resin cement (Super-Bond, Sun Medical, Japan) with the adjacent tooth (#46) for 1 month, with adjustments made to remove occlusal force from the tooth (Figures 3-5).

Figure 3. The tooth germ of #48 was extracted with the dental follicle in the cervical region.
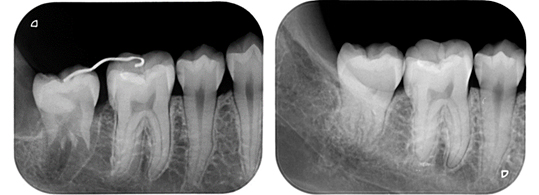
Figure 4. Immediately after transplantation procedure. The donor tooth was splinted to the adjacent tooth using a rectangular wire and resin cement.
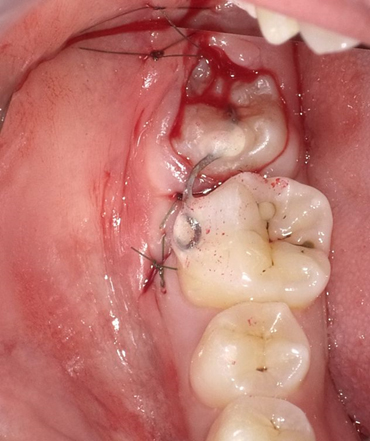
Figure 5. Dental X-ray findings. Left: Immediately after surgery. Right: Three years after surgery.
An Electric Pulp Test (EPT) (SybronEndo, Yoshida Co., Tokyo, Japan) was done after removal of tooth fixation. From the period of fixed removal to 5 years after the surgical procedure EPT test results were consistently negative. No root canal treatment was performed, as the pulp cavity showed shape changes in dental X ray examinations. At 3 years after the operation, no periodontal problems were observed, while the transplanted tooth was found to have migrated in a mesial and occlusal plane direction, with contact between adjacent teeth and occlusal contact with the opposite tooth observed. EPT findings remained negative, though the transplanted tooth showed good function. According to the past report, the success criterions after treatment are no clinical signs and symptoms of infection and inflammation around the donor teeth, no pain and no sensitivity to percussion, no root resorption and no ankylosis on X-ray examination was observed [7]. On the basis of success criteria, this case was in good success.
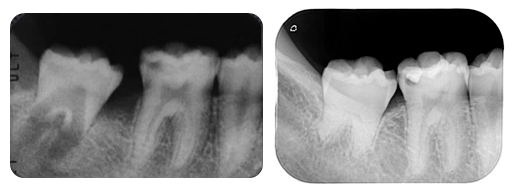
Dental Ⅹ-ray images of 4 other cases of auto transplantation performed in young patients are shown in (Figures 6-9). Good function was obtained in each of these cases and no periodontal problems were observed, though EPT findings were negative in all at each examination.
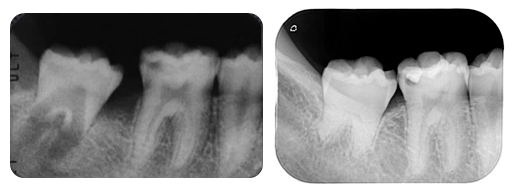
Figure 6. Male, 17 years old. The donor tooth germ (#48) was transplanted in the #47 site.
Left: Immediately after surgery. Right: Seven years after surgery.

Figure 7. Male, 14 years old. The donor tooth germ (#28) was transplanted in the #26 site.
Left: Immediately after surgery. Right: Three years after surgery.
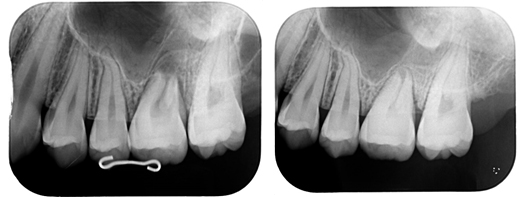
Figure 8. Female, 19 years old. The donor tooth germ (#28) was transplanted in the #26 site.
Left: Immediately after surgery. Right: Five years after surgery.

Figure 9. Male, 15 years old. The donor tooth germ (#28) was transplanted in the #36 site.
Left: Immediately after surgery. Right: Six years after surgery.
One of the main advantages of auto-transplantation is that it can be performed as treatment in a child during the growth period. Although few reports regarding tooth germ transplantation have been presented and the potential outcomes remain unclear, it is considered appropriate to use such a technique for patients with a missing tooth, such as the present cases. Tooth survival rates after 5 years of up to 90% have been reported with this procedure [8-10]. Nevertheless, to increase the possibility of a successful outcome, auto-transplantation requires use of meticulous candidate selection criteria, including factors such as general health, psychological state, and oral hygiene status. Furthermore, the recipient site should have sufficient bone support as well as an adequate amount of attached keratinized tissue to allow for tooth stabilization, and also no inflammation or infection [11].
Following oral surgery, the present patients required no additional treatment and only follow-up observations. Regarding pulp vitality, we were not able to confirm vital signs in any of the 5 cases using EPT. However, Mainkar et al. previously reported the efficacy of Doppler and pulse oximetry tests to detect pulp vital signs indicating calcified narrowed tooth pulp [12]. Furthermore, Gonzales et al., reported transient apical breakdown following tooth trauma or orthodontic treatment [13], and noted that affected teeth did not show vital signs in an EPT, though usually recovered to a normal condition within 1 year, thus no treatment other than monitoring was needed for their patients. In the present cohort, following the procedure, we were unable to confirm pulp vital signs with an EPT without the presence of symptoms such as radiographic evidence of root resorption or apical radiolucency. These issues require future investigation, as it may be possible to accurately detect vital signs using Doppler and pulse oximetry testing.
Even though EPT results were negative for all of the transplanted teeth in our cases, we did not perform root canal treatment, as there were no symptoms related to function and no pathological findings indicating the need for such treatment. Furthermore, the shape of the root pulp in each changed in X ray images obtained during the follow-up examinations. As for the transplanted donor teeth, sensitivity decreased over time because of calcification and narrowing of the dental pulp induced by an ischemic-reperfusion reaction following extraction [14]. Therefore, in addition to a sensitivity test, X-ray findings showing dental pulp form changes are reliable for determining whether a root canal procedure is needed.
Chiego et al. reported a case of severe injury to the pulpal neurovascular bundle. They noted that differences in chronological patterns of neural and vascular repair could lead to losing control of sympathetic nerve stimulation over odontoblastic secretory activity, resulting in rapid deposition of dentin and obliteration of the pulpal lumen [15]. We considered that the same process occurred in the present cases. With that point in mind, it would not be possible to avoid root canal obliteration following the present auto-transplantation procedures because a surgical technique was used. Thus, it is important to consider the difficulty of possible root canal treatment should that be indicated as necessary.
Following tooth transplantation, tooth migration in the mesial and occlusal plane direction was observed in each of the present cases. Morrees et al. reported that a transplanted tooth germ has a capability of auto eruption, especially during the early root development stage [16]. In consideration of tooth migration that occurs after the operation, the donor tooth should be placed at a level lower than the occlusal plane and covered with a muco-periosteal flap as much as possible to avoid infection of the root surface. Transplantation of an immature donor tooth and placing it at the height of the infra-occluded predecessor allows for continued eruption and encourages alveolar bone growth. Those processes have occurred in the present patients, with improved bone margins seen. Continued eruption will result in equalization of bony margins, resulting in good aesthetics.
In all 5 of the present cases of auto-transplantation in young patients, no clinical signs or symptoms of infection or inflammation have been seen in follow-up examinations performed 3 to 7 years after the oral surgical procedure. In addition, no pain or sensitivity to percussion, and no root resorption or ankylosis have been noted. Follow-up radiography examinations during the 3- to 7-year follow-up periods have revealed bone healing at the site of the previous peri radicular radiolucency (recipient site) as well as the presence of a continuous PDL space along the entire root surface. Based on our findings, tooth germ transplantation using an impacted third molar is considered to be an attractive alternative for treatment of a missing tooth in young patients.
Although high rates of success have been reported with auto-transplantation, a small number of cases fail. In those, the auto-transplant functions as an ideal natural space maintainer and preserves alveolar bone level, gingival tissue, and space in the dental arch. If the auto-transplant can be maintained until dentoalveolar maturation and patient growth cessation, then the recipient site may be more suitable for a future restorative option, such as dental implants, hence reducing the need for extensive pre-implant preparations.
Although the number of cases in this report is small, auto transplantation using an impacted third molar is suggested to be an alternative method for treatment of a lost molar in a young patient. We will continue to follow the present cases and report long-term results.
- Baseggio W, Naufel FS, Davidoff DC, Nahsan FP, Flury S, et al. (2010) Caries-preventive efficacy and retention of a resin-modified glass ionomer cement and a resin-based fissure sealant: a 3-year split-mouth randomized clinical trial. Oral health & preventive dentistry. 8:261-268. [Crossref]
- Sugai T, Yoshizawa M, Kobayashi T, Ono K, Takagi R, et al. (2010) Clinical study on prognostic factors for auto transplantation of teeth with complete root formation. International journal of oral and maxillofacial surgery. 39:1193-1203. [Crossref]
- Bolin AK, Bolin A, Jansson L, Calltorp J (1997) Children's dental health in Europe. Swedish dental journal. 21:25-40. [Crossref]
- Gill DS, Lee RT, Tredwin CJ (2001) Treatment planning for the loss of first permanent molars. Dental update. 28:304-308. [Crossref]
- Mendes RA, Rocha G (2004) Mandibular third molar auto-transplantation--literature review with clinical cases. Journal (Canadian Dental Association). 70:761-766. [Crossref]
- Hernandez SL, Cuestas-Carnero R (1988) Autogenic tooth transplantation: a report of ten cases. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 46:1051-1055. [Crossref]
- Zakershahrak M, Moshari A, Vatanpour M, Khalilak Z, Jalali Ara A. (2017) Autogenous Transplantation for Replacing a Hopeless Tooth. Iranian endodontic journal. 12:124-127. [Crossref]
- Andreasen JO, Paulsen HU, Yu Z, Ahlquist R, Bayer T, et al. (1990) A long-term study of 370 auto-transplanted premolars. Part I. Surgical procedures and standardized techniques for monitoring healing. European journal of orthodontics. 12:3-13. [Crossref]
- Andreasen JO, Paulsen HU, Yu Z, Bayer T. (1990) A long-term study of 370 auto-transplanted premolars. Part IV. Root development subsequent to transplantation. European journal of orthodontics. 12:38-50. [Crossref]
- Andreasen JO, Paulsen HU, Yu Z, Schwartz O. (1990) A long-term study of 370 auto-transplanted premolars. Part III. Periodontal healing subsequent to transplantation. European journal of orthodontics. 12:25-37. [Crossref]
- Kumar R, Khambete N, Priya E 2013 Successful immediate auto-transplantation of tooth with incomplete root formation: case report. Oral surgery, oral medicine, oral pathology and oral radiology. 115:16-21. [Crossref]
- Mainkar A, Kim SG (2018) Diagnostic Accuracy of 5 Dental Pulp Tests: A Systematic Review and Meta-analysis. Journal of endodontics. 44:694-702. [Crossref]
- Gonzalez OL, Vera J, Orozco MS, Mancera JT, Gonzalez KV, et al. (2014) Transient apical breakdown and its relationship with orthodontic forces: a case report. Journal of endodontics. 40:1265-1267. [Crossref]
- Yamaguchi S, Shibata R, Yamamoto N, Nishikawa M, Hibi H, et al. (2015) Dental pulp-derived stem cell conditioned medium reduces cardiac injury following ischemia-reperfusion. Scientific reports. 5:16295. [Crossref]
- Chiego DJ, Jr., Avery JK, Klein RM (1987) Neuroregulation of protein synthesis in odontoblasts of the first molar of the rat after wounding. Cell and tissue research. 248:119-123. [Crossref]
- Moorrees CF, Fanning EA, Hunt (1963) EE AGE VARIATION OF FORMATION STAGES FOR TEN PERMANENT TEETH. Journal of dental research. 42:1490-1502. [Crossref]