Alpha amylase is a well characterized carbohydrate splitting enzyme produced mainly in the parotid and submandibular salivary glands of humans and many other mammals. Apart from its role in the carbohydrate digestion, the salivary alpha amylase (sAA) has been given a possible role in the physiological and pathological activities taking place on the tooth surfaces, e.g. pellicle formation, bacterial adhesion and caries development. In addition, in the later years psychological research has revealed another property of sAA, that of being a stress biomarker reflecting increased catecholamine activity of the sympathetic nerve system. The stress based sAA is parallel with the salivary cortisol release along the HPA axis resulting in adrenal cortex stimulation, but the two biomarkers act independently. Experimental stress exposure of physical and psychological nature, sometimes combined with different psychopathological disorders, has evidenced this role of sAA. The easy access of saliva as compared with blood plasma, makes sAA a useful medium for stress evaluation without physical intervention. Obstacles for routine use of sAA as a stress biomarker are variations in amylase concentration, possibly caused by parasympathetic activity, and the lack of agreed methodology for collection and testing.
Amylase; Cathecolamine Activity; Stress Biomarker
Alpha amylase (alpha-1,4-glucan 4-glucanohydrolase, EC 3.2.1.1) is an enzyme hydrolyzing the bond between glucose repeats in starch, giving the disaccharide maltose, some glucose, and some units containing branching linkages other than the alpha-1,4 glucosidic linkage. In the animal kingdom the salivary amylase enzyme has been detected in some herbivores and many omnivorous animals, but not pure carnivores. Negligible or no salivary alpha amylase is present in ruminants. Nutritional habits may affect the expression of enzymes in the saliva of animals, genetically or epigenetically determined (1).
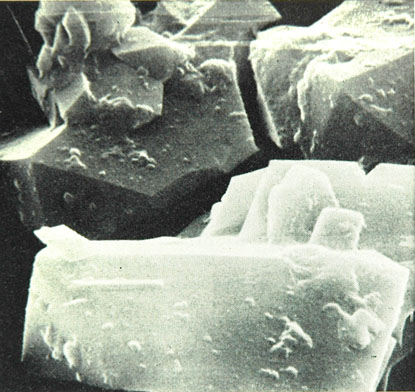
The human salivary alpha amylase (sAA) is produced mostly in the parotid glands, some in the submandibular glands, and small portions also in the sublingual and small salivary glands. The enzyme is exceptionally stable at high pH and temperature ranges. It has been purified and the amino acid composition determined many years ago, see Figure 1,2.The amylase activity in saliva has a diurnal profile pattern consisting of a distinct decrease within 60 minutes of awakening and then a steady increase of activity during the day (3). The physiological function of salivary sAA is to initiate the breakdown of starch in the oral cavity, continuing in the acid-protected parts of the food bolus during the gastric passage. Pancreatic alpha amylase finishes the breakdown in the duodenum. Here, the gut enzymes split the disaccharides to monosaccharides that may be absorbed by the intestines (4).
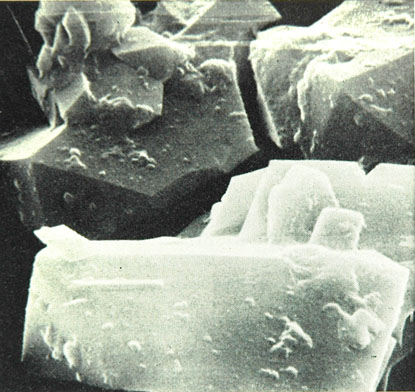
Figure 1. Scanning Electron Microscopy of Crystalline Alpha-Amylase form the Parotid Saliva of one Individual, obtained by Ammonium Sulfate-Acetone Precipitation. Reprint from our publication in Scandinavian Journal of Dental Research 1970 (reference no. 2) by permission of Wiley Global Permissions
Human salivary alpha amylase is present in the proteomics of the acquired dental pellicle, forming a complex with mucins and retaining part of its enzymatic activity. The amylase binds to several species of streptococci, facilitating their adherence to dental surfaces. It has been argued that sAA may provide breakdown products from starch that are metabolized by cariogenic bacteria and therefore is a factor in the caries etiology (5, 6). However, an early review (1972) concluded that sAA most probable was of minor importance in the caries etiology, since some clinical trials before that time showed a correlation and some did not (4). Over the years this pattern of clinical research has continued, some contemporary trials indicating a positive correlation between sAA and dental caries (7) and others showing the opposite (8). However, during the last 20 years psychological research has revealed a new aspect of the sAA: that of its function as a stress biomarker. The present survey aims at an update on this function of human salivary alpha amylase.
Salivary Biomarkers of Stress Response
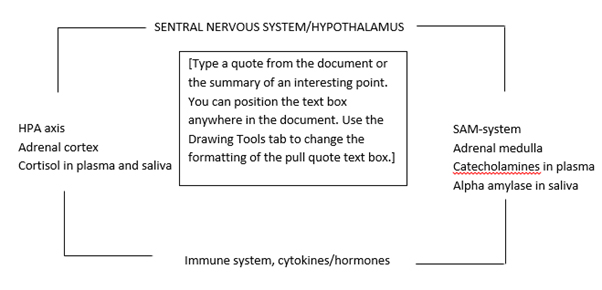
Physical and emotional stress has a physiologic impact by way of the autonomic nervous system. One pathway is the sympathetic adrenal medullary axis (SAM) in which the sympathetic nervous system (SNS) initiates the release of catecholamines (adrenaline and noradrenaline) from the adrenal medulla, leading to the “fight or flight” response with increased blood flow to brain, heart, muscles etc. (9).
The protein content of the saliva, including alpha amylase, is regulated by the SNS, whereas the fluid secretion is stimulated by the parasympathetic part of the autonomous nervous system (PNS) by the neurotransmitter acetylcholine. For this reason the salivary concentration of amylase may reflect stress-related SNS activity. CHATTERTON et al. (1996) demonstrated that both physical and mental stress showed an association between salivary alpha amylase and the plasma catecholamines: Increased noradrenaline and adrenaline in blood plasma induced by aerobic exercise was paralleled by increased alpha amylase in saliva, and examination stress showed a similar pattern with sAA and noradrenaline. Observations of this kind indicated the potential of salivary alpha amylase as a non-invasive biomarker of the stress related plasma catecholamine level (10).
Another stress reaction pathway is the Hypothalamus-Pituitary Axis (HPA), starting with hypothalamic stimulation and ending in the stimulation of the adrenal cortex to release glucocorticoids such as cortisol, leading to stress reactions similar to those of SAM (9). Both stress inducing pathways are influenced by the immune system Figure 2. Cortisol diffuses through the tissues and becomes part of the saliva. Alpha amylase and cortisol could therefore both be salivary indicators of stress response, avoiding stressful venipuncture that may confound the results of psychological stress tests. However, the salivary cortisol response is less sensitive and the recovery to pretask level is slower as compared to the alpha amylase. The sensitivity of sAA to psychosocial stress and the kinetic profile makes it of particular value as a potential stress biomarker (11).
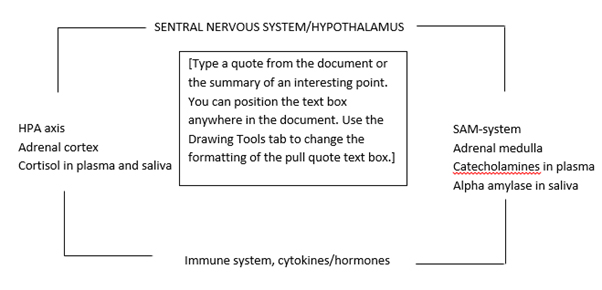
Figure 2. Simplified Illustration of Cooperating Stress Reaction Systems. To the right: The Sympathetic- Adrenal Medullary System (SAM). Fast working Effects by the Catecholamines Adrenaline and Noradrenaline in Blood. Increases Alpha Amylase in Saliva. To the left: The Hypothalamus - Pituitary- Adrenocortical axis (HPA). Increases Cortisol in Blood and Saliva. More Slow and Lasting Action. Under: The Stress Reactions are impacted by Cytokine and Peptide Hormones of the Immune System. The Connection line indicates that the three Stress Reaction Systems Communicate and Interact
Salivary Alpha Amylase in Psychophysiology and Psychopathology
Employing sAA as a biomarker in physiological stress conditions has been of great interest in psychophysiological research. Animal and human studies have shown raised sAA concentration as a response to stimulation of the beta-adrenergic receptors by SNS catechol activity. And inversely, this effect has been inhibited by beta blockers such as propranolol. There is no one to one correlation between the sympathetic neurotransmitter noradrenaline and the salivary alpha amylase, but a relationship is evidenced by the fact that exposure to a standardized psychosocial stress test such as the Trier Social Stress Test (TSST), leads to marked increase of many stress indicators including alpha amylase. An example is the association between sAA and cardiovascular parameters of the SNS, such as heart rate. The sAA measurements are considered to be of particular value as an indicator of SNS dysregulation in cases of anxiety (12). The TSST test comprises a job interview and an arithmetic task in front of an audience (13).
In recent years, many researchers have pursued the interest in sAA as a stress biomarker. Salivary alpha amylase increase has been demonstrated in response to physical and mental exposures such as venipuncture (14), viewing a video of eye surgery (15), and using the TSST test in a stress intervention study on military recruits with regard to a potential effect of physical fitness on psychosocial stress. Their reactions were evaluated by heart rate and sAA measurements after endurance run. Strong performance at the run proved to be a predictor of lower autonomous nerve system response as evidenced by the sAA level and the heart response curves (16).
Moreover, patients diagnosed with chronic psychosocial stress after detailed subjective and objective evaluation by expert psychologists have shown significantly elevated sAA as compared to patients without. Also, there was a significantly higher level of sAA in patients having oral complaints such as recurrent aphthous ulcers or dry mouth, whether they belonged to the stress group or not. The findings were interpreted as salivary alpha amylase being a biomarker for psychosocial stress but not an indicator to suggest stress related mucosal changes (17). An elevated pattern of sAA was also seen in sexually abused girls with posttraumatic stress disorder (PTSD). Together with other symptoms such as hyperarousal, flashbacks, nightmares etc., the sAA elevation in PTSD patients was interpreted as an indication of increased SNS activity in this group of patients (18).
Other clinical experiments have focused on the sAA variation associated with performance deficits after sleep loss. Over two days, total sleep loss resulted in increasingly poor experimental driving performance, not always coordinated with subjective feeling of sleepiness. On the other hand the diurnal profile of salivary alpha amylase was similar to performance, with levels peaking in the afternoon and declining in the evening and early morning. The association between salivary amylase and performance was explained by the role of noradrenergic activity affecting both factors. These findings highlighted the potential of sAA for assessing fitness for duty prior to safety in cases of sustained wakefulness (19).
However, other authors have cautioned that sympathetic activity should not be considered the only autonomous nerve factor in the alpha amylase secretion. Parasympathetic nerves also take part in this regulation. It is argued that collection methods of saliva, flow rate and stimulated or non-stimulated conditions are important factors that may influence the results together with a number of stimuli connected with digestion, speech and immune function (20).
Comparison of Salivary Alpha Amylase and Cortisol as Salivary Biomarkers
The relationship between the two stress biomarkers has been investigated by many psychologists in very different settings. Research in the time period 2007-2012 indicates that the interest for sAA as a non-invasive marker for sympathetic activity is growing. Apart from changes in sAA related to stress induced reactions in healthy subjects, dysregulation of the SAM system is associated with mental disorders such as general anxiety, panic or posttraumatic stress disorder, and possibly other psychopathology. It is assumed that stress reactions by the SAM system, expressed by aAA, and by the HPA system, expressed by cortisol, function in a coordinate manner, although the mechanisms ,e.g. additive or interactive, opposing or complementary, are unclear (21).
FURLAN et al. (2012) studied salivary cortisol and amylase in 7-8 year old children without dental treatment experience undergoing dental prophylaxis. There were higher cortisol and amylase levels in stimulated saliva before prophylaxis than afterwards, although no correlation between the two was found. The findings were interpreted as the result of pretreatment anticipation. The conclusion was that both ingredients were valuable and independent biomarkers for evaluating anxiety producing events. The sAA level was correlated with other SAM regulated reactions such as heart rate (HRT). The authors indicate that the amylase level may be of importance in evaluation of strategies for managing uncooperative child patients (22).
Other clinical trials in children included assessment of social anxiety followed by exposure to painful experiences such as cold, pressure, or heat, while unstimulated salivary samples before the exposure, immediately after, and 20 minutes after were tested for alpha-amylase activity and cortisol by enzymatic activity (sAA) or immunoassay (cortisol). Children reporting higher levels of social anxiety demonstrated elevated levels of salivary sAA at all testing times compared to children with low social anxiety scores. The findings were interpreted as sAA being an important marker of ANS activity in individuals sensitive to social evaluation. No such effect was seen on salivary cortisol, capturing more acute stress responses. Salivary alpha amylase therefore could be useful for identifying children at risk for stress (23). On the other hand, experimental evidence based on arithmetic stress loading showed that chewing reduced the stress reaction as seen by the decreased level of salivary cortisol, but not the sAA. The results indicated that chewing reduced the endocrine reaction system to mental stress (24).
Both biomarkers were employed in a crossover study on memory recall relative to two age groups (mean age 21 and 62 years) exposed to the TSST stress test consisting of free speech and a arithmetic task in front of an audience. Salivary cortisol and sAA were tested at several intervals before, during and after the procedures. Moreover, each participant performed a standardized memory test. The cortisol level increased after the stress task and then decreased, showing similar reaction in both age groups. The sAA level was also elevated by stress regardless of age, but reached pretask level more rapidly. The older group demonstrated a predominance of sAA stress response over cortisol, in combination with reduced immediate memory performance, emphasizing the function of sAA as a stress biomarker (25).
Tinnitus is regarded as a significant source of chronic stress. ALSALMAN et al (2016) studied the salivary stress response as evaluated by sAA, cortisol, and the immune system biomarker neopterin during a TSST test of a group of individuals with tinnitus and a group without. No significant effect was noticed on salivary cortisol or neopterin, but the tinnitus group had a lower level of sAA in general, remaining stable throughout the test. The lowered level of sAA was interpreted as an impaired sympathetic activity in tinnitus patients (26).
Another group of patients with enlarged stress level are breast cancer survivors constantly fearing recurrence. The stress response following TSST test in this group of patients have shown elevated diurnal and acute patterns of alpha amylase compared to healthy women, whereas the salivary cortisol has shown normal diurnal pattern and a blunted acute pattern. These results were interpreted as an effect of allostatic disruption of the two stress regulating systems, demonstrating different reaction patterns. According to the researchers these findings illustrate the complexity of the relationship between the two stress reaction systems and need further clarification (27).
Repeated stress situations such as childhood maltreatment may be accompanied by psychopathologies of different kind. The diurnal salivary alpha amylase and cortisol have been tested among adolescent boys with externalizing problems such as conduct disorder, oppositional defiant disorder, and ADHD. The values followed a normal pattern, showing a high cortisol concentration in the morning, lower at midday and lowest at evening, whereas the salivary alpha amylase was low in the morning and higher at midday and evening i.e. fairly normal. Boys with conduct disorders (bullying, threatening, theft, intimidation etc.) had a lower sAA activity as compared with other groups. According to ANGYAL et al. (2016) this finding could be used to characterize subgroups of individuals with externalizing problems (28).
Using the Trier Social Stress Test MIELOCK et al. (2017) found increased cortisol reactivity in women who had been maltreated in childhood, followed by rapid slowing down of the cortisol level. These women showed no stress effect on the salivary alpha amylase level, as opposed to non-maltreated women in the control panel. The missing amylase effect was unexpected, as elevated sAA has been detected in adolescent girls with posttraumatic stress disorder after sexual abuse (18). One explanation offered was that the parasympathetic nervous system participated along with the sympathetic activity in maltreated women (29).
COSMA et al. (2017) has evaluated stress studies with emphasis on cardiovascular effects using a-amylase and cortisol as clinical indicators. The overall finding was that salivary a-amylase and cortisol both could be considered a potential tool for detecting stress induced cardiac disease, provided that strict methodological protocols were followed (30).
Table 1 gives an impression on different approaches employed by some researchers to elucidate the relationship between and stress and salivary alpha amylase as a biomarker: straight clinical observation of stress condition, experimental stress exposure, and experimental exposure of psychopathological patient groups.
Table 1. Some Studies on Elevated Salivary Alpha Amylase as a Stress Biomarker
Author, Year, Reference No
|
Stressors
|
Study Design
|
FURLAN et al. 2012, ref. 22
|
Predental treatment anticipation
|
Observational psychological trial
|
VINEETHA et al. 2014, ref. 15
|
Psychosocial stress
|
Observational psychological trial
|
KEESHIN et al. 2015, ref. 16
|
Posttraumatic stress disorder
|
Observational psychological trial
|
KOH et al. 2014, ref. 12
|
Venipuncture
|
Experimental psychological trial
|
SAHU et al. 2014, ref. 13
|
Video of surgery
|
Experimental psychological trial
|
WYSS et al. 2016, ref.14
|
Psychosocial stress test
|
Experimental psychological trial
|
PAJCIN et al. 2017, ref. 19
|
Sleep loss
|
Experimental psychological trial
|
PAYNE et al. 2014, ref. 23
|
Social anxiety and pain exposure
|
Observational and experimental psychological trial
|
HIDALGO et al. 2014, ref. 25
|
Psychosocial stress test and age
|
Observational and experimental psychological trial
|
WAN et al. 2016, ref. 27
|
Psychosocial stress test on breast cancer survivors
|
Observational and experimental psychological trial
|
ANGYAL et al. 2016, ref. 28
|
Psychosocial stress test on mal-treated boys
|
Observational and experimental psychological trial
|
ASALMAN et al. 2016, ref. 26*
|
Psychosocial stress test on tinnitus victims
|
Observational and experimental psychological trial
|
MIELOCK et al. 2017, ref. 29*
|
Psychosocial stress test on mal-treated women
|
Observational and experimental psychological trial
|
Finishing Remarks
The abundance of alpha amylase in saliva and the easy testing procedures are factors contributing to many theories over the years of its role in oral physiology and pathology, e.g. such as pellicle formation, bacterial adhesion, and caries etiology. The present overview deals with another factor emerging during the last two decades, that of sAA being a non-invasive stress biomarker representing the catechol effect of the sympathetic medullary axis of the autonomous nerve system (SAM). The increased stress related sAA secretion is paralleled by cortisol increase initiated by the HPA axis and leaking into the saliva along with other plasma components. Salivary cortisol and sAA are independent tools for non-invasive estimation of acute and chronic stress levels in patients, but their different diurnal secretion patterns and their functions are not synchronized.
Most issues in this area are associated with psychopathology and research work of this nature is published in psychology related journals. The reports referred to above are selected to give an excerpt of recent research shedding light on the topic of sAA as a stress biomarker for the dentistry oriented reader. Most reports show that acute stress and stress present in chronical psychopathological disorders demonstrate increased alpha amylase in saliva as part of an increased protein release. Researchers agree that sAA is considered an indicator of increased sympathetic nervous system activity as part of other of stress induced salivary components such as chromogranin and heat shock proteins (31). The increased sAA as a response to psychological and physical stress tests on healthy individuals and on individuals with psychosocial disorders has been regarded as a diagnostic possibility distinguishing between certain psychopathological disorders.
However, quantitative variations in the sAA stress response are not uncommon, one deviant factor being the possibility that parasympathetic activity may modify the otherwise sympathetic based amylase secretion (20). In addition, practical considerations such as the diurnal pattern of sAA secretion, the mode of collection of saliva, and lack of standardized testing kits are obstacles to be addressed before routine clinical use.
- Lindsten R, Kurol J (1997) Orthodontic appliances in relation to nickel hypersensitivity: a review. Journal of Orofacial Orthopedics 58(2): 100–108. [Crossref]
- Starkjaer L, Menne T (1990) Nickel allergy and orthodontic treatment. European Journal of Orthodontics 12(3): 284–289. [Crossref]
- Shelley BW (1981) Gingival hyperplasia from dental braces. Cutis 28(2):149–150. [Crossref]
- Bishara SE , Barrett RD , Selim M (1993) Biodegradation of orthodontic appliances. Part II. Changes in the blood level of nickel. American Journal of Orthodontics and Dentofacial Orthopedics 103(2): 115–119. [Crossref]
- Eliades T , Trapalis C , Eliades G , Katsavrias E (2003) Salivary metal levels of orthodontic patients: a novel methodological and analytical approach. European Journal of Orthodontics 25(1): 103–106. [Crossref]
- Holmstrup P (1999) Non-plaque induced gingival lesions. Annals of Periodontology 4(1): 20–29. [Crossref]
- Limberger KM, Westphalen GH, Menezes LM, Medina-Silva R (2011) Cytotoxicity of orthodontic materials assessed by survival tests in Saccharomyces cerevisiae. Dental Materials 27(5): e81–e86. [Crossref]
- Shigeto N, Yanagihara T, Hamada T, Budtz-Jørgensen E (1989) Corrosion properties of soldered joints. Part I: electrochemical action of dental solder and dental nickel-chromium alloy. The Journal of Prosthetic Dentistry 62(5): 512–515. [Crossref]
- Mockers O, Deroze D, and Camps J (2002) Cytotoxicity of orthodontic bands, brackets and archwires in vitro. Dental Materials 18(4): 311–317. [Crossref]
- Berge M, Gjerdet NR, Erichsen ES (1982) Corrosion of silver soldered orthodontic wires. Acta Odontologica Scandinavica 40(2): 75–79. [Crossref]
- Fleischer M, Sarofim AF, Fassett DW, Hammond P, Shacklette HT, et al. (1974) Environmental impact of cadmium: a review by the panel on hazardous trace substances. Environmental Health Perspectives 7: 253–323. [Crossref]
- Novelli ELB, Hernandes TR, NovelliFilho JLVB, Barbosa LL (1998) Differential/combined effect of water contamination with cadmium and nickel on tissues of rats. Environmental Pollution 103(2-3): 295–300. [Crossref]
- Jin YH, Clark AB, Slebos RJC, Al-Refai H, Taylor JA, et al. (2003) Cadmium is a mutagen that acts by inhibiting mismatch repair. Nature Genetics 34(3): 326–329. [Crossref]
- Xie J, Shaikh ZA (2006) Cadmium induces cell cycle arrest in rat kidney epithelial cells in G2/M phase. Toxicology 224(1-2): 56–65. [Crossref]
- Huff J, Lunn RM, Waalkes MP, Tomatis L, Infante PF (2007) Cadmium-induced cancers in animals and in humans. International Journal of Occupational and Environmental Health 13(2): 202–212. [Crossref]
- Mikulewicz M, Chojnacka K (2011) Cytocompatibility of medical biomaterials containing nickel by osteoblasts: a systematic literature review. Biol. Trace Elem. Res 142: 865–889. [Crossref]
- Loe H, Theilade E, Jensen SB (1965) Experimental gingivitis in man. J Periodontol 36: 177-187. [Crossref]
- Ericsson I, Thilander B (1978) Orthodontic forces and recurrence of periodontal disease: An experimental study in the dog. Am J Orthod 74(1): 41-50. [Crossref]
- Ericsson I, Thilander B (1980) Orthodontic relapse in dentitions with reduced periodontal support: An experimental study in dogs. Eur JOrthod 2(1): 51-57. [Crossref]
- Ericsson I, Thilander B, Lindhe J, Okamoto H (1977) The effect of orthodontic tilting movements on the periodontal tissues of infected and non-infected dentitions in dogs. J ClinPeriodontol 4(4): 278-293. [Crossref]
- Polson AM, Subtelny JD, Meitner SW, Polson AP, Sommers EW, et al. (1988) Long-term periodontal status after orthodontic treatment. AmJ Orthod 93: 51-58. [Crossref]
- Amini F, Borzabadi Farahani A, Jafari A, Rabbani M (2008) In vivo study of metal content of oral mucosa cells in patients with and without fixed orthodontic appliances. Orthod Cranio fac Res 11(1):51-56. [Crossref]
- Kolokitha OE, Chatzistavrou E (2009) A severe reaction to Ni – containing orthodontic appliances. Angle Orthod 79(1): 186-192. [Crossref]
- Williams DF (2008) On the mechanisms of biocompatibility. Biomaterials 29(20): 2941–2953. [Crossref]
- Menezes LM, Quint˜ao CCA (2010) The release of ions from metallic orthodontic appliances. Seminars in Orthodontics 16(4): 282–292. [Crossref]
- Menezes LM, Campos LC, Quint˜ao CC, Bolognese AM (2004) Hypersensitivity to metals in orthodontics. American Journal of Orthodontics and Dentofacial Orthopedics126(1): 58–64. [Crossref]
- Andresen GF, Morrow RE (1978) Laboratory and clinical analyses of nitinol wire. Am J Orthod 73(2): 142–151. [Crossref]
- Schuster G, Reichle R, Bauer RR, Schopf PM (2004) Allergies induced by orthodontic alloys: incidence and impact on treatment. Results of a survey in private orthodontic offices in the Federal State of Hesse, Germany. J Orofac Orthop 65(1): 48–59. [Crossref]
- Eliades T (2007) Orthodontic materials research and applications: Part 2: current status and projected future developments in materials and biocompatibility. Am J Orthod Dentofacial Orthop 131(2): 253–262. [Crossref]
- Pereira BR, Tanaka OM, Lima AAS, Guariza-Filho O, Maruo H, et al. (2009) Metal and ceramic bracket effects on human buccal mucosa epithelial cells. Angle Orthod 79(2): 373–379. [Crossref]
- Malkoc S, Corekci B, Ulker HE, Yalçin M, Sengün A (2010) Cytotoxic effects of orthodontic composites. Angle Orthod 80(4): 759–764. [Crossref]
- Toy E, Malkoc S, Corekci B, Bozkurt BS, Hakki SS (2014) Real-time cell analysis of the cytotoxicity of orthodontic brackets on gingival fibroblasts. J Appl Biomater Funct Mater 12(3): 248 -255. [Crossref]